What Is Ventricular Fibrillation?
When someone dies suddenly, a dangerous heart arrhythmia called ventricular fibrillation (VF) is often the cause. Recognizing the signs of VF can save lives.
Arrhythmias are abnormal heart rates or rhythms. They can be totally benign, over quickly, and have simple explanations. For example, if you are almost hit by a speeding car, your body pumps out adrenaline, and your heart rate likely increases to a far greater than normal rate. Fear can also trigger out-of-sync skipped beats; so can lack of sleep or stimulants. But some arrhythmias need treatment. One, ventricular fibrillation, is often deadly.
In fact, ventricular fibrillation (also called VF or V-fib) is the most serious cardiac rhythm disturbance, according to the American Heart Association (AHA).
It’s the primary cause of sudden cardiac arrest, a life-threatening emergency that occurs when you heart suddenly stops beating. It can strike people of all ages who may appear to be healthy, even children and teenagers, the Sudden Cardiac Arrest Foundation points out.
YOU MIGHT ALSO LIKE: Implantable Defibrillators Help Older Patients Live Longer
Understanding ventricular fibrillation
When a famous person dies suddenly and unexpectedly, sometimes the death is immediately reported in the news as a heart attack. While heart attacks may trigger VF, however, ventricular fibrillation and heart attacks are two different things.
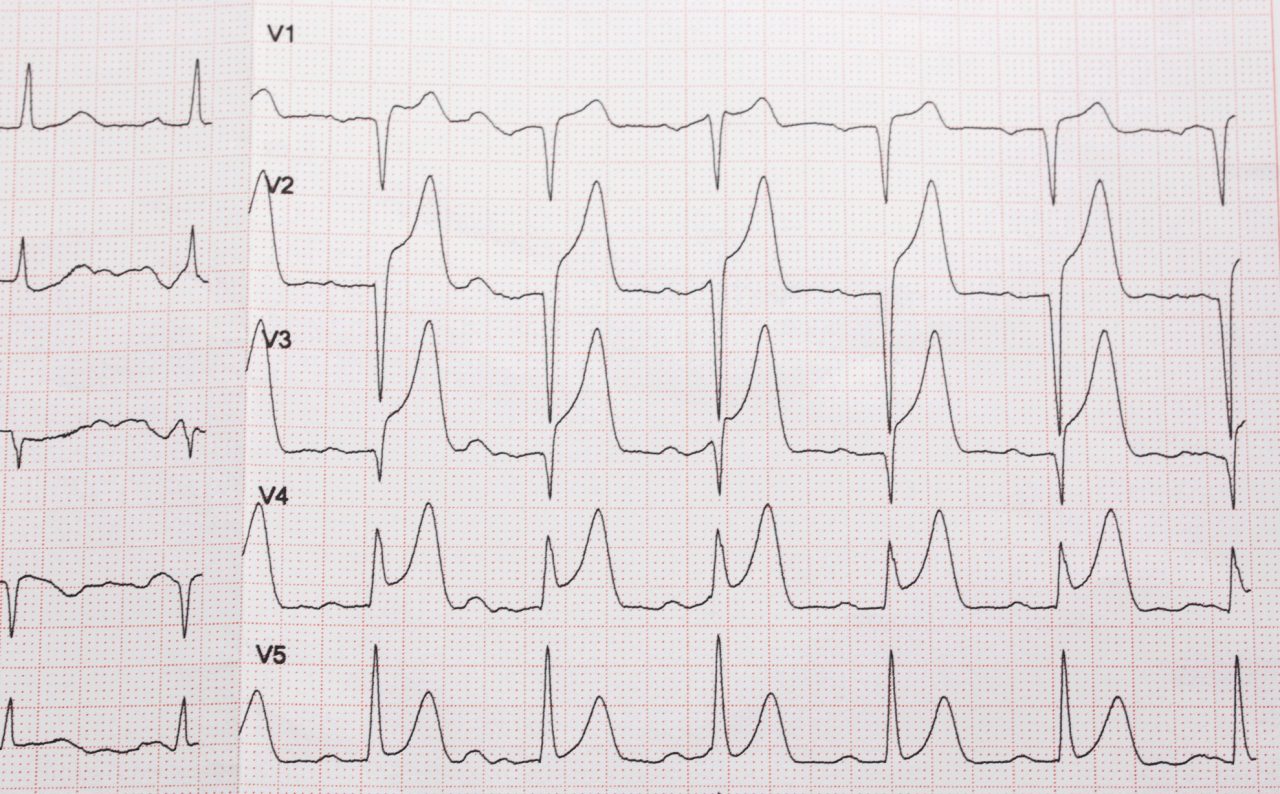
In cardiology lingo, fibrillation refers to a rapid, irregular heart rate. Atrial fibrillation occurs in the upper chambers of the heart (the atria) and shouldn’t be confused with ventricular fibrillation.
Although atrial fibrillation can be dangerous if untreated, primarily because it raises your risk of blood clot-caused strokes, it is generally not life-threatening. Ventricular fibrillation, on the other hand, occurs in the lower chambers of your heart (the ventricles) and disrupts its ability to pump any blood at all.
In VF, disorganized electrical signals make the ventricles quiver instead of pumping blood to your body. Without immediate emergency care, sudden cardiac arrest and death typically occur within a few minutes, according to the National Heart, Lung and Blood Institute (NHLBI).
It’s important to note that not all ventricular arrhythmias signal VF. For example, premature ventricular beats are common and, unless they’re very frequent, simply mean your heart is skipping beats in the lower chambers of your heart.
Ventricular fibrillation risk factors
Ventricular tachycardia is a fast, regular beating of the ventricles. It can occur for only a few seconds and may not cause any other problems. The NHLBI points out, however, ventricular tachycardia that lasts for more than a few seconds can be dangerous, causing fainting or triggering life-threatening ventricular fibrillation.
Seek medical attention for symptoms of ventricular tachycardia:
- Chest pain
- Rapid heartbeat over 100 beats per minute, with no explanation
- Dizziness
- Nausea
- Shortness of breath
- Fainting
In addition to ventricular tachycardia, risk factors for ventricular fibrillation include damage to your heart muscle (from a heart attack, for instance), disease of the heart muscle (such as cardiomyopathy), or heart failure, which impacts your heart’s pumping ability.
A viral infection of the heart, sepsis (a severe bacterial infection that releases organ-harming toxins into your bloodstream), and reactions to prescription or recreational drugs can also cause ventricular fibrillation, the AHA notes.
Coronary artery disease and related risk factors — smoking, high blood pressure, diabetes, high cholesterol, obesity, and a sedentary lifestyle — are also risk factors. Significant changes in blood levels of potassium and magnesium, most often from taking diuretics, can trigger VF, too.
How to help people survive ventricular fibrillation
According to the Sudden Cardiac Arrest Foundation, over 350,000 Americans experience ventricular fibrillation every year outside of a hospital setting — often with no warning while they are going about their business at work, shopping, or at home. Without immediate help, death will occur within minutes.
If you see someone who suddenly collapses and is not breathing or only gasping and does not respond to tapping on the shoulder, treat this as a likely sudden cardiac death event. Follow these steps recommended by the AHA:
- Immediately call 911 for help. Or yell for someone nearby to call while you attend to the person.
- Ask another bystander to bring you an AED (automated external defibrillator). They are typically automatic and do not need special training to use; follow the prompts on the machine. AEDs are frequently available at airports, malls, and in police cars.
- Check breathing. If the person isn’t breathing, or is only gasping, administer CPR until an AED or emergency help arrives.
- Administer CPR. If you are not trained, visit the AHA Hands-only CPR page to learn a simple, life-saving CPR emergency technique.
- Keep pushing. Continue administering CPR until the person starts to breathe or move, until someone with more advanced training takes over, or until a someone with an AED or emergency personnel arrives.
Prevention and treatment of VF
If a person survives a ventricular fibrillation episode, the risk of sudden death remains high unless there is immediate treatment. Almost always, a defibrillator is implanted that shocks the heart to stop ventricular fibrillation or ventricular tachycardia (which may trigger VF) when it occurs.
Many people with ventricular fibrillation or ventricular tachycardia also are prescribed antiarrhythmic drugs to reduce the odds of future ventricular tachycardia and ventricular fibrillation events.
Cardiac ablation (a procedure that uses heat or extreme cold to eliminate cells in the heart causing the arrhythmia) can cure VF for many people, reducing or eliminating their risk factors.
Updated:
March 09, 2023
Reviewed By:
Janet O’Dell, RN