What Is Cardiac Catheter Ablation?
Cardiac catheter ablation, a minimally invasive procedure, can treat a variety of irregular heart rhythms, including atrial fibrillation and other arrhythmias.
Millions of Americans have an arrhythmia, which means the rate or rhythm of their heartbeat is too fast, too slow, or irregular. Arrhythmias can come and go, while others are persistent. Some may cause anxiety and be mistaken for panic attacks but are not life threatening. But other arrhythmias, depending on the type, can raise your risk of stroke and even result in sudden death.
Medication can often help calm arrhythmias and pacemakers, and implanted defibrillators can control the most serious forms of abnormal heart rhythms. For an increasing number of heart arrhythmia patients, however, minimally invasive cardiac catheter ablation (also called catheter ablation) can cure their erratic heart rhythm.
YOU MIGHT ALSO LIKE: What Is Atrial Fibrillation?
Understanding your heart’s electrical system and arrhythmias
To understand cardiac catheter ablation, it’s important to consider your heart’s own electrical system. The power source that keeps your heart beating originates in the upper right chamber of your heart (the right atrium) at the sinoatrial (SA) node.
The SA node works much like a “natural pacemaker,” the American Heart Association points out. It’s composed of cells that generate electrical impulses that travel through the upper chambers of your heart to the atrioventricular (AV) node, the heart’s electrical relay station between the upper and lower chambers of the heart. The AV node sends the electrical impulses down to a group of specialized fibers called the His-Purkinje system and into all parts of the ventricles (the heart’s lower chambers).
If the electrical impulse is transmitted normally, your heart pumps and beats at a regular pace. If something disrupts or blocks the electrical impulses, your heart may develop a brief and temporary, sporadic, or long-lasting arrhythmia.
During the past decades, advances in technology have helped electrophysiologists (cardiologists who specialize in diagnosing and treating arrhythmias) to zero in on exactly what kind of abnormal heart rhythm a person has — and the origin of electrical glitches.
For a growing number of patients with arrhythmias, cardiac catheter ablation can be the treatment of choice. In fact, in many cases, it can be curative.
What is cardiac catheter ablation?
Depending on a person’s diagnosis, medical history, and other factors, if an electrophysiologist determines catheter ablation could potentially cure a heart rhythm problem, an electrophysiology (EP) study is typically performed in a hospital, immediately prior to an ablation. This test can document exactly what cells in the heart are responsible for irregular or fast heartbeats and exactly where the cells are located, the National Heart, Lung and Blood Institute (NHLBI) explains.
An EP study and ablation involve catheters guided through a blood vessel, usually in the groin or upper thigh, via high-tech imaging, to the heart. An electrophysiologist precisely guides a catheter, which contains tiny electrodes, as it records and locates the source of the abnormal heartbeats.
To ablate the cells causing the arrhythmia, the electrophysiologist aims the tip of a special catheter at a small area of heart tissue containing the troublesome cells. Then a machine sends either radiofrequency waves, extremely cold temperatures, or laser light through the catheter to create a scar called an ablation line. The result is a minute barrier that halts abnormal electrical signals from traveling to the rest of the heart and causing arrhythmias.
The patient is checked after the procedure with an EKG and, depending on health and other factors, may be sent home soon after the procedure, with no hospital stay. The patient will need follow up visits with a cardiologist to make sure the ablation was successful.
While ablations are not without risks, they are considered very low risk when a highly experienced electrophysiologists performs them. What’s more, the procedure can cure many arrythmias.
Who can benefit from cardiac catheter ablation?
Sometimes an arrhythmia is linked to heart disease, congenital problems, reactions to drugs, smoking, or injuries to the heart, or there may not be any known specific explanation.
Some people have no symptoms during an arrhythmia (and the irregular heartbeat may be discovered accidentally during a physical). Others many feel it when their heart is beating irregularly or too quickly. Some people may feel faint or dizzy or have shortness of breath during an arrhythmia.
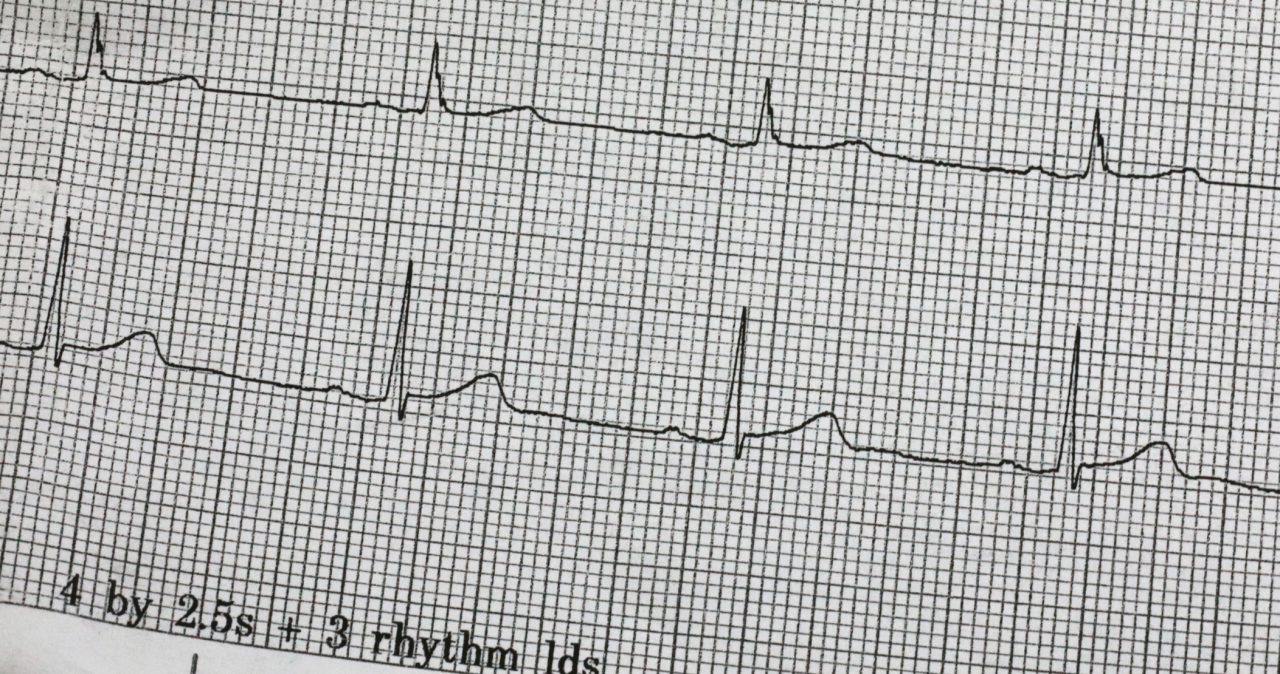
If a person is experiencing an ongoing arrhythmia, a doctor will perform an electrocardiogram (abbreviated as EKG or ECG). Painless electrodes temporarily attached to their body measure the electrical activity of the heartbeat and record whether it is fast, slow, or irregular. In addition, by measuring how much electrical activity is passing through the heart muscle, the EKG can help a cardiologist determine if the heart is enlarged.
Some arrhythmias, however, occur only now and then and may not show up on the EKG. You can wear small monitors (Holter monitors that can record EKG activity for 24 hours) or postage stamp-sized loop recorders implanted just under your skin. Those devices can help catch and record arrhythmias that seem to come and go, sometimes with weeks or months of normal heart rhythm in between episodes of erratic beats. Your doctor may also have you take a treadmill (exercise) test.
Types of arrythmia cardiac catheter ablation can treat
- AV nodal reentrant tachycardia (AVNRT). This arrhythmia results from an extra pathway in or near the AV node, which can erratically cause the electrical impulse to move in a circle and re-enter areas of the heart it already passed through. The result is palpitations and tachycardia (a heart rate over 100 beats per minute).
- Paroxysmal supraventricular tachycardia (PSVT). A usually benign arrhythmia, a PSVT can strike out of the blue and is often misdiagnosed as a panic attack. It involves erratic electrical activity in the upper heart chamber that can cause the heart to beat 100 to 200 beats per minute. (A normal adult resting heart rate ranges from 60 to 100 beats per minute.) Episodes of PSVT, as well as AVNT, may last for only a few minutes and usually stop on their own, but they need treatment in the ER if they continue for an hour or more.
- Atrial Fibrillation and atrial flutter. Extra electrical signals originating in different parts of the upper chambers of the heart (atria) can cause the heart to beat very rapidly (atrial flutter) or quiver (atrial fibrillation, also called afib). Although some patients report no symptoms, many suffer from palpitations, fatigue, and shortness of breath. Atrial fibrillation is the most common arrhythmia in the U.S., affecting almost three million Americans. If not treated adequately (usually with several prescription medications, including anticoagulants), it raises your risk of stroke and congestive heart failure.
- Ventricular tachycardia. This arrhythmia can be lethal and cause sudden, unexpected deaths. It is marked by a rapid, potentially life-threatening rhythm originating from impulses in the lower chambers (ventricles) that block the heart from filling with adequate blood to circulate through the body.
Can you avoid a cardiac ablation procedure?
Medication, often taken for the rest of your life, can help atrial fibrillation symptoms and reduce their chances of triggering a stroke, without having a cardiac catheter ablation. A study by the NHLBI found patients who were treated with ablation reported much greater symptom relief and long-term improvements in their quality of life, including fewer recurrences of the condition and fewer hospitalizations, than those treated only with medication.
YOU MIGHT ALSO LIKE: Our Heart Care section
Updated:
May 25, 2022
Reviewed By:
Janet O’Dell, RN