Cases of Late-Stage Cervical Cancer Are Rising
White women in their 40s in the South are seeing yearly increases in deadly late-stage cervical cancer, which is preventable with vaccinations and screenings.
Advanced cervical cancer is a rare illness with limited treatment options. Sadly, only 17 percent of patients survive for five years after their diagnosis, and the number of cases is rising among American women. But we could be preventing more of these illnesses.
Nearly 30,000 women in the United States were diagnosed with a late-stage cervical cancer from 2000 to 2018, with rates rising 1.3 percent each year. Black women have more than 60 percent higher risk than white women, but the risk is growing most quickly — at a rate of 4.5 percent a year — among white women aged 40 to 44 in the South.
Nearly 90 percent of all cases are linked to human papillomavirus (HPV), the most common sexually transmitted disease in the United States. Researchers point out that many young women aren’t vaccinated against HPV, and nearly 27 percent of white women miss screening through gynecological tests.
YOU MIGHT ALSO LIKE: Why You Need Screening for Cervical Cancer
Risk factors for cervical cancer
You are more at risk of this kind of cancer if you become sexually active before the age of 18, have many partners, or have a partner who has an HPV infection or has had many partners. Using birth control pills for many years increases your risk (an IUD may lower it). A chlamydia infection may help HPV grow. Women who smoke double their risk (tobacco byproducts have been found in the cervix).
Women who become pregnant before the age of 20 and women who have three or more full-term pregnancies may be vulnerable. People who take immunosuppressant drugs should talk to their doctors about special precautions.
What you can do
The best way to avoid cervical cancer is to get vaccinated against HPV. Vaccination can protect you for years. But only 66 percent of white teenagers ages 13 to 17 are vaccinated. It’s best to get vaccinated before the age of 27. You can still opt for HPV vaccination between ages 27 and 45, but by then you may already have been exposed to the virus.
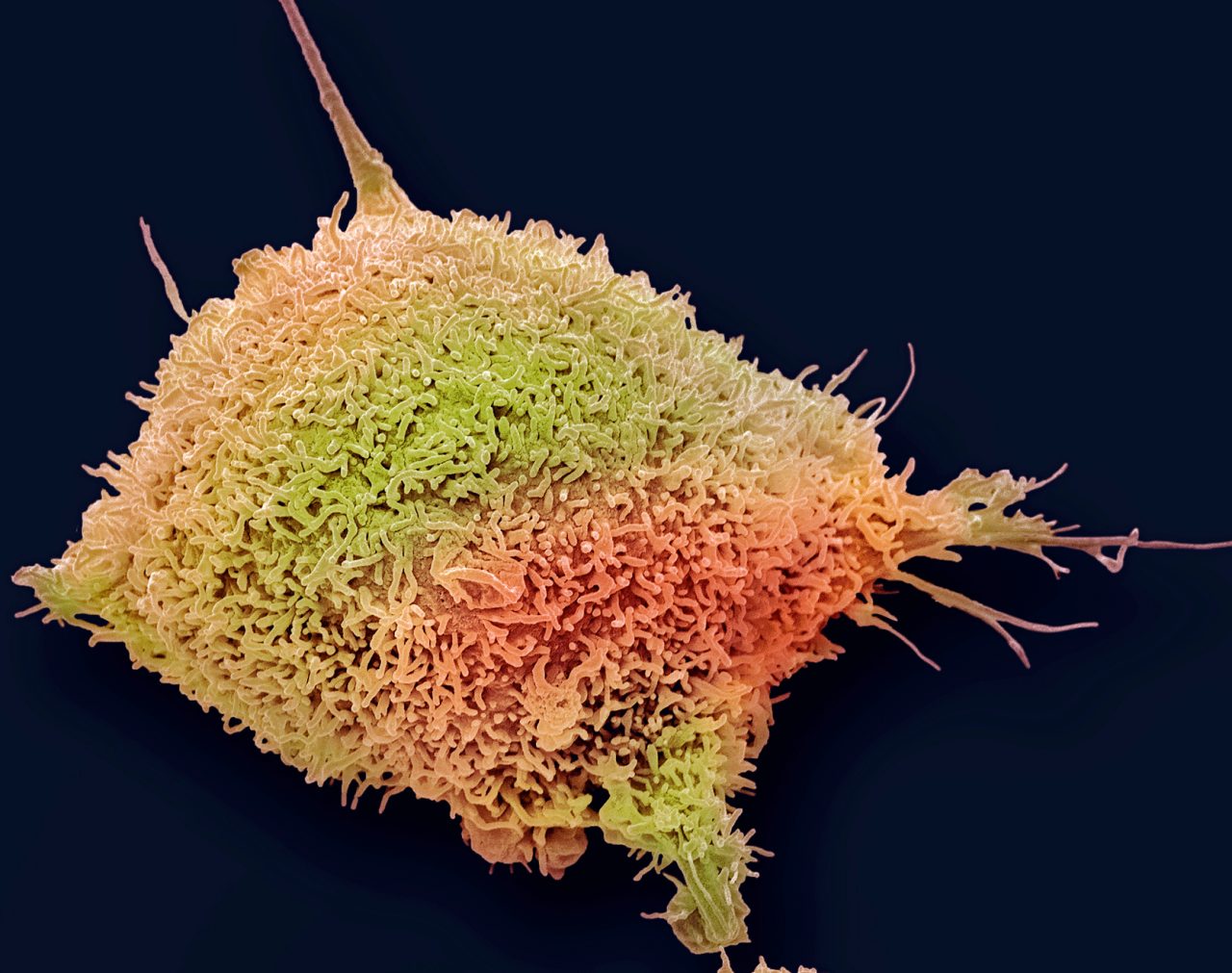
Screenings can include an HPV test or Pap smear, when cells from the surface of the cervix are viewed under a microscope.
The American Cancer Society (ACS) recommends the HPV test every five years for everyone with a cervix from age 25 until age 65. Another option is a HPV/Pap co-test every five years or a Pap test every three years.
Catching the cancer early makes a huge difference.
Note that the ACS changed its recommendations in 2020, dropping Pap tests for women in their early 20s and endorsing five-year intervals.
Talk to your gynecologist about the right screening for you. You may think your risk of catching HPV is low because you don’t have sex or have sex only in a monogamous relationship. But you might fall into the small group that develops cervical cancer for another reason or your partner may have caught HPV through sex since your last test.
Don’t panic if you hear that you have HPV. These infections are common and, in most people, the body clears the infection without treatment. Moreover, there are different kinds of HPV, and only some are classified as high-risk.
Updated:
December 09, 2022
Reviewed By:
Janet O'Dell, RN