Symptoms of Exocrine Pancreatic Insufficiency
These serious symptoms are overlooked, yet they’re connected to many diseases. Here's what you should know about exocrine pancreatic insufficiency.
Julie DuBois has chosen to be a voice of people with exocrine pancreatic insufficiency (EPI), which interferes with digestion and can cause malnutrition.
Dubois is a dietitian and elite personal trainer with EPI. She has celiac disease and ulcerative colitis. But it was chronic pancreatitis that triggered the EPI.
EPI, which is difficult to diagnose, a can be a complication of pancreatitis, cystic fibrosis, irritable bowel disorder, diabetes, and other autoimmune diseases.
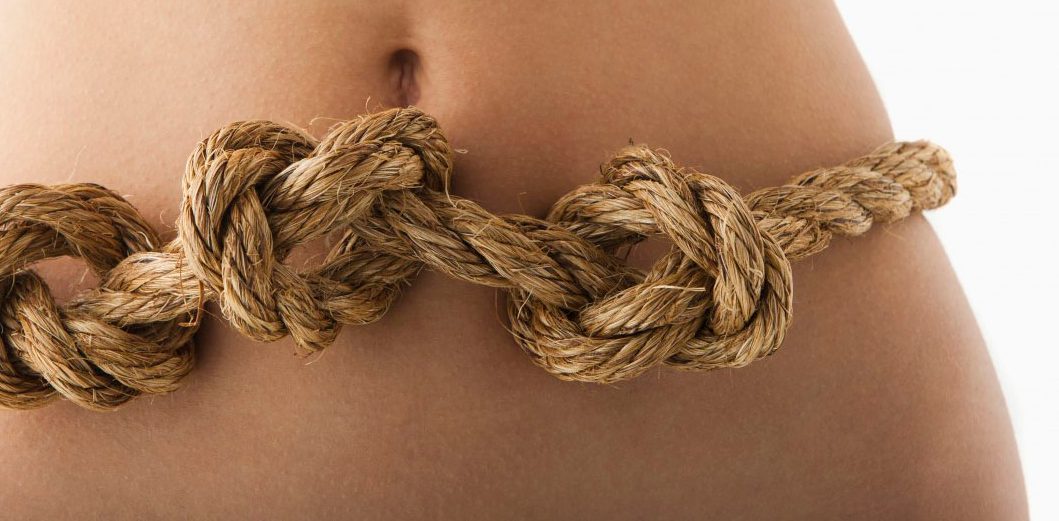
When their intestines can’t absorb nutrients from food, people with EPI may end up with bone loss and gastrointestinal problems, including weight loss, nausea, loss of appetite, gas, bloating, and steatorrhea (loose stools with unabsorbed fat).
YOU MIGHT ALSO LIKE: What Is Lactose Intolerance?
If you have EPI, you know it’s more than just unpleasant. It’s potentially dangerous, raising your risk of cardiovascular disease and other illnesses.
Dubois was diagnosed with EPI in 2011 and has talked about building bathroom breaks into her ballet classes to avoid unfortunate consequences.
People with chronic pancreatitis like DuBois are at the greatest risk for EPI. Over years of living with the disease, the inflammation can lead to irreversible damage to the pancreas, including the cells that secrete pancreatic digestive enzymes. These enzymes are important in nutrition, as they break down carbohydrates, fats, and protein for your body to use.
If you have the symptoms that characterize EPI, don’t let them fester.
Testing for diagnosis of exocrine pancreatic insufficiency is widely available. It is possible to take enzymes to increase your ability to absorb nutrients.
Dubois keeps a food journal to document what’s she’s eating and the calories those foods contain. She also records symptoms that seem to be associated with certain foods. That journal helps her, and can help you, fine-tune your diet in consultation with your doctor.
She has the advantage of being a dietitian, making her more familiar with what her food options are. But you can educate yourself over time to learn that as well.
Extra measures of support for your gastrointestinal (GI) system include stress reduction and plenty of sleep. Dubois says both affect her GI symptoms, for better or worse.
Generally, you want to avoid dehydration, which can worsen EPI symptoms. Also, ease into a low-fat diet. Less fat could help lead your bowel movements back to regularity and lessen, if not eliminate, stools that are far more unpleasant than usual.
A study of Japanese patients with chronic pancreatitis and steatorrhea found that it occurs less and is milder in that population because their fat intake is lower than that of Americans and Europeans.
You’re still going to need some healthy fats in your diet so you can metabolize mineral supplements and fat-soluble vitamins A, D, E, and K. You need them all. That’s where your doctor or dietitian can help you choose which foods are best for you.
A high-fiber diet may be good for most of us. For people with EPI, however, it could lead to more gas and flatulence, a study found. Again, if you have EPI, talk to you doctor about how much fiber you need and how much you can actually ingest.
Another tip: Don’t smoke or drink. Of course, both habits are bad for your general health since they increase the risk of heart disease and cancer. They’re also not friendly to the pancreas.
EPI stays under the radar for a couple of main reasons. One, its symptoms may not seem distinct to you from the disease that causes it. Two, it's not pretty. But, now that you know what it involves, acknowledge it and get help.
Updated:
July 21, 2022
Reviewed By:
Janet O’Dell, RN