What Is Deep Vein Thrombosis?
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein. It’s important to understand DVT prevention and symptoms because DVT can be deadly.
It may seem like you are perfectly safe, working at your desk daily for many hours on end or sitting on a plane, happily traveling on a smooth flight to a vacation in a faraway land. Or maybe you’re recovering from a successful operation, taking it easy for a few weeks on the couch. All of these scenarios can put you at risk for a medical condition — deep vein thrombosis (DVT) — that can cause serious, and even deadly, complications.
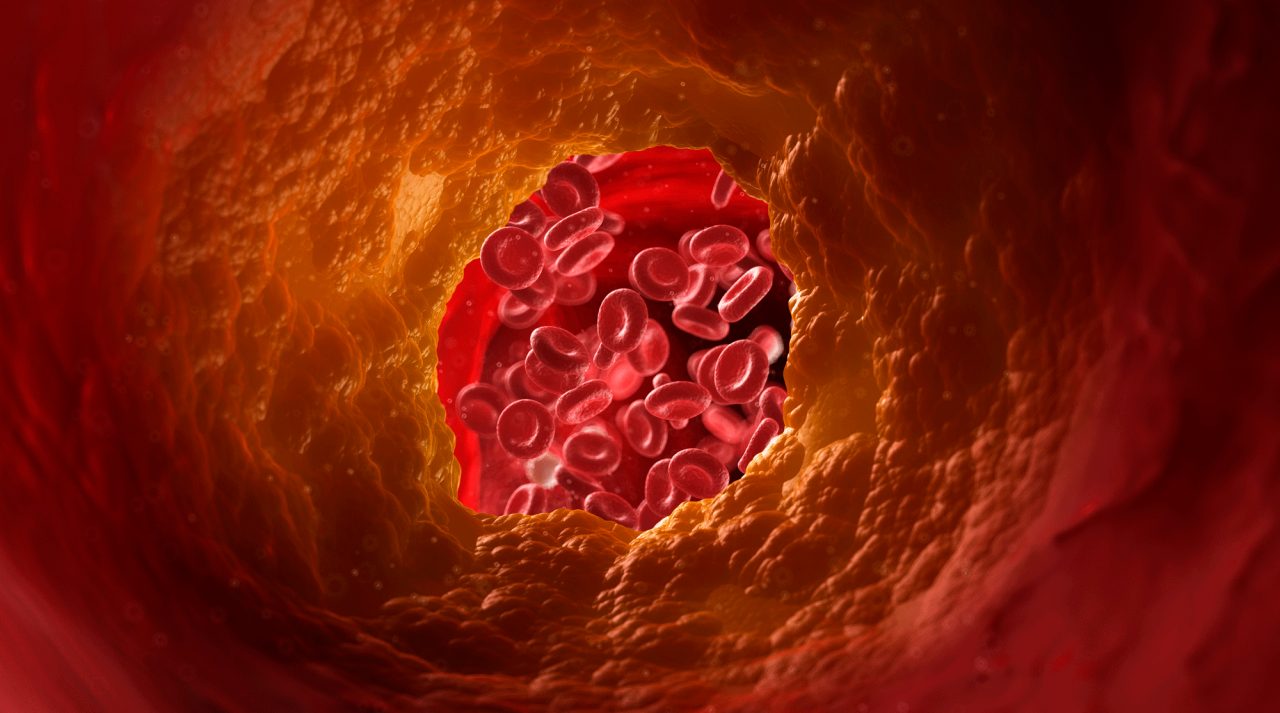
To understand deep vein thrombosis (DVT), consider what the term means: A thrombosis is a blood clot that occurs in a deep vein. Usually DVT develops in a lower leg, thigh, or pelvis, but a thrombosis can also sometimes develop in an arm.
It’s important to know what deep vein thrombosis is because, while certain risk factors and lifestyle changes can help prevent the condition, DVT can happen for unknown reasons. Recognizing the symptoms and getting help quickly if you spot DVT signs is crucial to avoid potentially serious complications that can lead to pain, disability, and sometimes death, the Centers for Disease Control and Prevention (CDC) points out.
YOU MIGHT ALSO LIKE: Signs and Symptoms of a Blood Clot
CDC statistics show DVT is far more common than many people realize. For example, while precise numbers of cases are not known, as many as 900,000 Americans annually may experience the condition. What’s more, estimates show that about 60,000 to 100,000 Americans die each year due to DVT or a complication from the blood clot.
Deep vein thrombosis risk factors
Although DVT occurs sometimes in people with no known risk factors, many medical conditions and lifestyle factors can place you at risk.
Not exercising and being sedentary at your work or during a long trip raise the risk. DVT can also happen if you are confined to your bed or a chair for weeks after an accident or surgery, or even when you break a bone and have to wear a cast.
The National Heart Lung and Blood Institute (NHLBI) explains, when there is a lack of physical movement, blood slows through the veins in your legs and arms, raising DVT risk. This creates a low oxygen situation, resulting in more clot formation, especially in veins deep in your calves.
Other deep vein thrombosis risk factors
- An injury to veins from an accident or surgery can cause clots to form.
- Being significantly overweight or obese raises pressure in legs and the pelvic area, upping the risk for blood clots.
- Pressure on veins in a woman’s pelvis and legs during pregnancy raises the risk of DVT, with the risk lasting up to six weeks after giving birth.
- Birth control pills and hormone replacement therapy can result in blood clotting more easily.
- Smoking is linked to an increased risk of DVT because it increases blood clotting and hampers circulation.
- Several health conditions put you at increased deep vein thrombosis risk, including heart failure, inflammatory bowel diseases (such as Crohn’s disease and ulcerative colitis), and certain types of cancer.
- A family or personal history of DVT raises the chances of experiencing a deep vein blood clot.
- Growing older is a risk factor you can’t change. After age 40, the risk of DVT almost doubles every decade, according to the NHLBI.
We can’t emphasize this enough: DVT can be life-threatening
Deep vein thrombosis symptoms aren’t the same for everyone who experiences the condition. Sometimes DVT doesn’t cause noticeable symptoms until serious complications occur.
On the other hand, deep vein thrombosis often causes pain and a cramping or sore sensation near the blood clot. An affected part of the body, usually a leg (especially the calf), may swell and become red or discolored. The area may also feel unusually warm.
One potential complication of DVT is post-thrombotic syndrome (PTS), caused by poor blood flow, inflammation, and blood vessel damage from a blood clot in a deep vein. PTS is a long-lasting condition and can be disabling, according to the NHLBI. In addition to pain, swelling, and discoloration, PTS can cause itchiness, cramping, and fatigue, and the symptoms often worsen if you have to stand or walk for an extended period. Sometimes, skin sores develop.
A pulmonary embolism is another serious complication of deep vein thrombosis – and it can be deadly. It’s the result of a blood clot breaking loose, moving through your bloodstream, and lodging in your lungs. Symptoms include sudden shortness of breath, feeling light-headed or fainting, rapid pulse, coughing up blood, and chest pain or discomfort that hurts more when you cough or take a deep breath. These are warning signs to call 911 and seek emergency care.
Not everyone with DVT experiences a serious complication or needs treatment, but you do need to be under the care of a physician. In some cases, if your doctor detects a clot, your condition may be monitored for only a while. However, anti-coagulant drugs to stop clots from becoming larger are typically prescribed.
Thrombolytics, medications that dissolve large blood clots causing severe complications (such as pulmonary embolism), are also used in treating DVT. Because these drugs can cause sudden bleeding, however, they are primarily used only for potentially life-threatening pulmonary embolisms.
For people who cannot take these drugs, a vena cava filter may be used to prevent a pulmonary embolism. The filter is inserted inside a large vein (the vena cava) to catch any blood clots before they move into the lungs. This prevents a pulmonary embolism.
How to lower the risks for deep vein thrombosis
The good news about DVT is that quick treatment can often avoid serious complications. In addition, there are ways you can be proactive to greatly lower your risk of deep vein thrombosis.
CDC Advice for DVT prevention
- Maintain a healthy weight and get regular exercise.
- Start moving after surgery, an injury, or illness, as soon as your doctor says it’s safe.
- If you’re at known risk for DVT, talk to your doctor about wearing graduated compression stockings or taking anticoagulant medication to help prevent deep vein thrombosis.
- If you have to sit for an extending period of time — for example, when traveling on a long trip — get up and walk around every two to three hours, even if all you do is walk up and down the aisle on a plane.
- You can also exercise your legs while sitting by raising and lowering your toes while keeping your heels on the floor; tighten and release your leg muscles, too.
Updated:
September 24, 2021
Reviewed By:
Janet O’Dell, RN