Having Laparoscopic Cholecystectomy
Having Laparoscopic Cholecystectomy
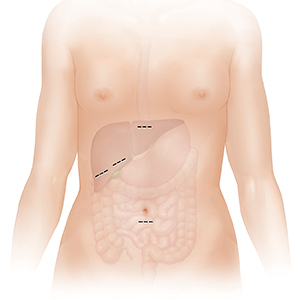
Small incisions are made in your belly (abdomen). The scope is put through one of the incisions. Surgical tools are put through other incisions.
Small clips are used to close off the connection between the gallbladder and the bile duct. The gallbladder is then detached from the liver.
The gallbladder is removed through one of the incisions. Bile still flows from the liver to the small intestine.
When the surgery is done, all tools are removed. Incisions are closed with stitches (sutures) or staples. Sometimes, a laparoscopic surgery may need to be changed to an open surgery. This method uses one large incision. This change may happen because of scar tissue, unusual anatomy, or for some other reason.
You’ve had painful attacks caused by gallstones. Because of this, you are having surgery to remove your gallbladder. This is called cholecystectomy. A method called laparoscopy will be used. This allows surgery to be done through a few small cuts (incisions).
Before your surgery
-
Tell your provider what medicines you take. This includes prescription medicines, over-the-counter medicines, street drugs, herbs, vitamins, and other supplements. Be sure to mention if you take prescription blood thinners. This includes warfarin, clopidogrel, ibuprofen, and aspirin.
-
If you drink alcohol, tell your provider how much you drink. This is very important if you are a heavy drinker or have had alcohol withdrawal symptoms in the past. Alcohol withdrawal can be dangerous. But the symptoms can be safely managed if your healthcare provider knows your alcohol history.
-
Have any tests your provider asks for, such as blood tests.
-
Don’t eat or drink after midnight the night before your surgery. This includes water, coffee, and mints.
The day of surgery
-
Your provider may have you take your normal medicine with a sip of water. Check with your provider.
When you arrive, you will prepare for surgery:
-
An IV (intravenous) line will be put into a vein in your arm or hand. This gives you fluids and medicine.
-
An anesthesiologist will talk with you about anesthesia. This is medicine used to prevent pain. You will receive general anesthesia. This puts you into a deep sleep-like state through the procedure.
During laparoscopic surgery
For this surgery, a thin tube with a tiny camera is used. This is called a laparoscope.The scope sends images from inside your body to a video screen. This lets the surgeon view and work on your gallbladder:
-
Small incisions are made in your belly (abdomen). The scope is put through one of the incisions. Surgical tools are put through other incisions.
-
Small clips are used to close off the connection between the gallbladder and the bile duct. The gallbladder is then detached from the liver.
-
The gallbladder is removed through one of the incisions. Bile still flows from the liver to the small intestine.
-
When the surgery is done, all tools are removed. Incisions are closed with stitches (sutures) or staples. Sometimes, a laparoscopic surgery may need to be changed to an open surgery. This method uses one large incision. This change may happen because of scar tissue, unusual anatomy, or for some other reason.
After surgery
You will be sent to a room to wake up from the anesthesia. You will likely go home the same day. In some cases, an overnight stay is needed. When you are released to go home, have a family member or friend ready to drive you.
All surgeries have risks. The risks of gallbladder surgery include:
-
Bleeding
-
Infection
-
Injury to the common bile duct or nearby organs
-
Blood clots in the legs
-
Bile leaks
-
Hernia at incision site
-
Pneumonia
Updated:
March 15, 2019
Sources:
Cholangioscopy and Pancreatoscopy, UpToDate, Management of moderate and severe alcohol withdrawal syndromes. UpToDate.
Reviewed By:
Jen Lehrer MD