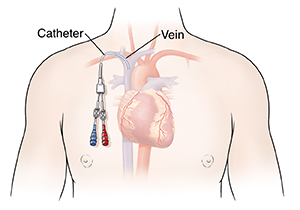
Discharge Instructions: Caring for Your Central Line
Discharge Instructions: Caring for Your Central Line
Understanding your role
A nurse or other healthcare provider will teach you and your caregivers how to care for the central line. Before leaving the hospital, make sure you understand what to do at home, how long you may need the central line, and when to have a follow-up visit.
You will likely be told to flush the central line with saline or heparin solution. You may also be told to change the catheter’s injection caps and change the bandage (dressing). Or, a nurse may do this for you during a follow-up visit. Only do these things if you’re told to do so. Follow the instructions you were given.
Protecting the central line
If the central line gets damaged, it won’t work right and could raise your chance of infection. Call your healthcare team right away if any damage occurs. To protect the central line at home:
Prevent infection. Use good hand hygiene by following the guidelines on this sheet. Don’t touch the catheter or dressing unless you need to. And always clean your hands before and after you come in contact with any part of the central line. Your caregivers, family members, and any visitors should use good hand hygiene, too.
Keep the central line dry. The catheter and dressing must stay dry. Don’t take baths, go swimming, use a hot tub, or do other activities that could get the central line wet. Take a sponge bath to avoid getting the central line wet, unless your healthcare provider tells you otherwise. Ask your provider about the best way to keep the line dry when bathing or showering. If the dressing does get wet, change it only if you have been shown how. Otherwise, call your healthcare team right away for help.
Avoid damage. Don’t use any sharp or pointy objects around the catheter. This includes scissors, pins, knives, razors, or anything else that could cut it or put a hole in it (puncture it). Also, don’t let anything pull or rub on the catheter, such as clothing.
Watch for signs of problems. Pay attention to how much of the catheter sticks out from your skin. If this changes at all, let your healthcare provider know. Also watch for cracks, leaks, or other damage. If the dressing becomes dirty, loose, or wet, change it (if you have been instructed to). Or call your healthcare team right away.
Avoid lowering your chest below your waist. This includes bending at the waist to do things like tying your shoes. When your chest is below your waist, especially for a long time, the catheter’s internal tip could slip out of place in the vein.
Tell your healthcare team if you vomit or have severe coughing. This can also make the catheter slip out of place.
Risk of blood clot
If a blood clot forms it can block blood flow through the vein where the catheter is placed. Signs of a blood clot include pain or swelling in your neck, face, chest or arm. If you have any of these symptoms, call your healthcare provider right away. You may need an ultrasound exam to find the blood clot. You may also be treated with a blood thinner.
Prevent infection with good hand hygiene
A central line can let germs into your body. This can lead to serious and sometimes deadly infections. To prevent infection, it’s very important that you, your caregivers, and others around you use good hand hygiene. This means washing your hands well with soap and water, and cleaning them with alcohol-based hand gel as directed. Never touch the central line or dressing without first using one of these methods.
To wash your hands with soap and water:
Wet your hands with warm water. (Avoid hot water. It can cause skin irritation when you wash your hands often.)
Apply enough soap to cover the entire surface of your hands, including your fingers.
Rub your hands together briskly for at least 15 seconds. Make sure to rub the front and back of each hand up to the wrist, your fingers and fingernails, between the fingers, and each thumb.
Rinse your hands with warm water.
Dry your hands completely with a new, unused paper towel. Don’t use a cloth towel or other reusable towel. These can harbor germs.
Use the paper towel to turn off the faucet, then throw it away. If you’re in a bathroom, also use a paper towel to open the door instead of touching the handle.
When you don’t have access to soap and water: Use alcohol-based hand gel to clean your hands. The gel should have at least 60% alcohol. Follow the instructions on the package. Your healthcare team can answer any questions you have about when to use hand gel, or when it’s better to wash with soap and water.
When to seek medical care
Call your healthcare provider right away if you have any of the following:
Pain or burning in your shoulder, chest, back, arm, or leg
Fever of 100.4°F (38.0°C) or higher
Chills
Signs of infection at the catheter site (pain, redness, drainage, burning, or stinging)
Coughing, wheezing, or shortness of breath
A racing or irregular heartbeat
Muscle stiffness or trouble moving
Gurgling noises coming from the catheter
The catheter falls out, breaks, cracks, leaks, or has other damage
Updated:
June 20, 2018
Sources:
Complications of central venous catheters and their prevention. UpToDate., Gorski. Central Venous Access Device Associated Infections: Recommendations for Best Practice in Home Infusion Therapy. Home Healthcare Nurse (2010); 28(4); pp. 221-227
Reviewed By:
Image reviewed by StayWell medical illustration team.,Mancini, Mary, MD,Ziegler, Olivia, MS, PA