Distal Ureterectomy
Distal Ureterectomy
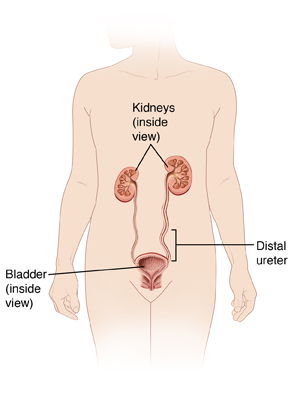
The ureters are tubes that connect and drain urine from the kidneys to the bladder. Cancer has been found in the lower (distal) part of one of your ureters. To treat the cancer, distal ureterectomy is done. This surgery removes the lower part of the ureter and part of the bladder.
Preparing for surgery
Prepare for the surgery as you have been told. In addition:
-
Tell your doctor about all medicines you take. This includes prescription, over-the-counter, herbs and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery, as directed by your doctor.
-
Don't eat or drink during the 8 hours before your surgery. This includes coffee, water, gum, and mints. (If you have been instructed to take medicines, take them with a small sip of water.)
Two types of surgery
The surgery may be done through several small incisions (laparoscopy). Or, it may be done through one larger incision (open surgery). Laparoscopy cannot be used in all cases. In some cases, your doctor may start surgery using laparoscopy but must change to open surgery for safety reasons. You and your doctor will discuss your options.
-
For laparoscopy, the doctor makes several small incisions in the abdomen. The scope is put through one of the small incisions. The scope sends pictures from inside the abdomen to a video screen. Surgical tools are placed through the other incisions. The surgeon may use a technique called robotic laparoscopy. The robotic system gives a 3D view inside the body. It also assists the surgeon’s hand movements.
-
For open surgery, one larger incision is made in the side. The doctor sees and works through this incision.
The day of surgery
The surgery takes about 2 to 3 hours. Afterward, you will stay in the hospital for 1 to 3 nights.
Before the surgery begins:
-
An intravenous (IV) line is put into a vein in your arm or hand. This line delivers fluids and medicines (such as antibiotics).
-
You may get medicine to prevent blood clots.
-
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine puts you into a state like deep sleep through the surgery. A tube may be inserted into your throat to help you breathe.
-
A thin tube (catheter) is placed into your bladder through the urethra. This drains urine during the surgery and for a time afterward.
During the surgery:
-
The area is checked for cancer spread. If any is seen the procedure may be stopped.
-
The lower end of the ureter and part of the bladder are removed. Nearby lymph nodes may also be removed. The remaining ureter is then reinserted into the bladder and sewn into place.
-
A long, flexible tube called a stent is put into the ureter. It reaches from the kidney into the bladder. It is kept in place for 4 to 6 weeks after surgery to help hold the ureter open while it heals.
-
The catheter may be left in the bladder, to drain urine while the bladder heals.
-
When the surgery is done, all tools are removed. The incision or incisions are closed with sutures, staples, surgical glue, or strips of surgical tape. One or more tubes (drains) may be placed into the incision site. These drain fluid that may build up as healing starts.
Recovering in the hospital
After the surgery, you will be taken to a recovery room where you will be monitored as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. When you are ready, you will be taken to your hospital room. While in the hospital:
-
You will be given medicine to manage pain. Let your providers know if your pain is not controlled.
-
The catheter in your urethra and any drains will likely be removed before you leave the hospital. If not, you will be told how to care for them at home.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days, to help care for you. Recovery time varies for each person. Your doctor will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Make sure to:
-
Take all medicines as directed.
-
Care for your incisions as instructed. If you’re sent home with a catheter or drains, take care of these as you were shown.
-
Follow your doctor’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incision to be covered with water until the doctor says it’s OK.
-
Don't do strenuous activity, as advised by your doctor.
-
Don't drive until your doctor says it’s OK. Don't drive if you’re taking medicines that make you drowsy or sleepy.
-
Don't strain during a bowel movement. If needed, take stool softeners as directed by your doctor.
The stent in your ureter will cause the urge to pass urine more often. You may also have some burning and blood in your urine. This is normal and will go away once the stent is removed during a follow-up visit.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Chest pain or trouble breathing (call 911)
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Bleeding or a large amount of drainage from an incision
-
Symptoms of infection at an incision site such as increased redness or swelling, warmth, worsening pain, or foul-smelling drainage
-
Large clots of blood in your urine
-
Pain or swelling in the legs
-
Pain that’s not controlled with medicine
-
Inability to urinate
-
Vomiting that doesn’t go away
Follow-up care
You will have follow-up visits with your surgeon. If sutures or staples need to be removed, this is done 7 to 14 days after surgery. The stent in your ureter will be removed in 4 to 6 weeks. You will also have regular follow-up visits with your doctor to be sure the cancer doesn’t return or spread. If any further cancer treatments are needed, your doctor can tell you more.
Risks and possible complications
-
Bleeding (may require a blood transfusion)
-
Infection
-
Urine leakage from the ureter or bladder
-
Stricture (narrowing) in the ureter
-
Damage to the bladder, bowels, or other organs
-
Blood clots
-
Kidney damage
-
Tumor seeding (spillage of tumor cells that can grow into new tumors)
-
Risks of anesthesia (the anesthesiologist will discuss these with you)
Updated:
March 16, 2019
Sources:
Surgical repair of an iatrogenic ureteral injury, Up To Date
Reviewed By:
Greenstein, Marc, DO,Sather, Rita, RN