Ureterolysis
Ureterolysis
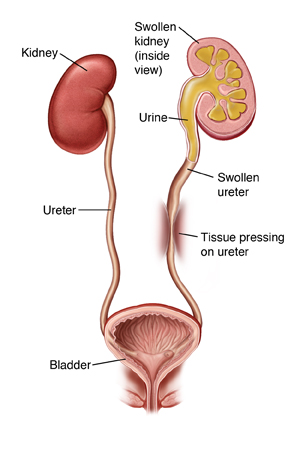
The ureters are tubes that carry urine from the kidneys to the bladder. Pressure from a mass of tissue or scar tissue is blocking one or both of your ureters. This causes urine to back up into the kidneys instead of flowing out of the body. Ureterolysis can help treat this problem. With this surgery, the ureter is freed from the tissue that is pressing on it. The ureter is then moved to a new position away from the blockage.
Two types of surgery
The surgery may be done through several small incisions (laparoscopy). Or it may be done through one larger incision (open surgery). Laparoscopy cannot be used in all cases. In some cases, your doctor may start surgery using laparoscopy but must change to open surgery for safety reasons. You and your doctor will discuss your options.
For laparoscopy, the doctor makes several small incisions in the abdomen. The scope is put through one of the small incisions. This sends pictures from inside the abdomen to a video screen. Surgical tools are placed through the other incisions. The surgeon may use a technique called robotic laparoscopy. The robotic system gives a 3D view inside the body. It also assists the surgeon’s hand movements.
For open surgery, one larger incision is made in the abdomen. The doctor sees and works through this incision.
Preparing for surgery
Prepare for the surgery as you’ve been told. In addition:
Tell your doctor about all medicines you take. This includes prescription, over-the-counter, herbs and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery, as directed by your doctor.
Don't eat or drink during the 8 hours before your surgery. This includes coffee, water, gum, and mints. (If you have been instructed to take medications, take them with a small sip of water.)
You may be given a special liquid or medicine to take the day before the surgery. This is to make sure your colon is empty for the surgery. Follow the instructions you are given.
The day of surgery
The surgery takes about 3 to 6 hours. You will stay in the hospital for 1 to 3 nights afterward.
Before the surgery begins:
An intravenous (IV) line is placed in a vein in your arm or hand. This supplies fluids and medicines such as antibiotics.
You may get medicine to prevent blood clots.
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine lets you sleep comfortably through the surgery. A tube may be inserted into your throat to help you breathe.
You may have an epidural to help control post-surgery pain. A small tube is inserted into your back to deliver pain medicine that numbs the lower body. Talk to your doctor or anesthesiologist about this option.
A thin tube (catheter) is placed into your bladder to drain urine.
During the surgery:
One or more incisions are made to access the ureters. The number of incisions depends on the method of surgery being used.
The ureter is freed from the tissue around it.
The cause of the blockage is removed, if possible. This may involve removing scar tissue or a mass that’s pressing on the ureter.
The ureter is moved to a new position that allows it to drain better. It is secured in place with stitches (sutures).
A thin tube (stent) may be placed in the ureter as it heals. The stent helps widen the ureter so urine can flow through it properly.
If needed, treatment is also done on the other ureter.
When the surgery is complete, all tools are removed. Any incisions made are closed with stitches or staples. In some cases, surgical glue or strips of surgical tape are used instead.
A small tube (drain) may be placed near the incision or incisions. This drains fluid that may build up after the surgery.
Recovering in the hospital
After the surgery, you will be taken to a recovery room where you will be monitored while waking up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. When you are ready, you will be taken to your hospital room. While in the hospital:
You will get medicine to manage pain. Let your providers know if your pain is not controlled.
The catheter and drain will likely be removed before you go home. If not, you’ll be shown how to care for them at home.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days, to help care for you. Recovery time varies for each person. Your doctor will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Make sure to:
Take all medicines as directed.
Care for your incisions as instructed.
Follow your doctor’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incision to be covered with water until your doctor says it’s OK.
Don't lift anything heavy or do strenuous activities, as directed.
Don't drive until your doctor says it’s OK. Don't drive if you’re taking medicines that make you drowsy or sleepy.
Walk a few times daily. Increase your pace and distance, as you feel able.
Don't strain to pass stool. If needed, take stool softeners as directed by your doctor.
Drink plenty of water. This helps prevent urine odor and dehydration. And follow any other diet instructions you’re given.
If stents were placed in your ureters, you’ll feel the urge to pass urine more often. You may also have some burning and blood in your urine. This is normal and will go away once the stents are removed during a follow-up visit.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
Chest pain or trouble breathing (call 911)
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
Symptoms of infection at an incision site such as increased redness or swelling, warmth, worsening pain, or foul-smelling drainage
Bloody urine with clots
Trouble urinating or no urination for 4 hours
Pain that cannot be controlled with medicines
Nausea or vomiting that won’t go away
Pain or swelling in the legs
Follow-up care
You’ll have follow-up visits so your doctor can check how well you’re healing. If your stitches or staples need to be removed, this will likely be done in 7 to 14 days. Stents will be removed in 2 to 6 weeks. Going forward, you may need regular visits with your doctor. During these visits, routine tests may be done to check how well your kidneys and ureters are working.
Risks and possible complications
Bleeding (may require a blood transfusion)
Infection
Blood clots
Urine leakage from one or both ureters
Blockage or scarring of one or both ureters recurs
Damage to the kidney, bladder, bowels, or other organs
Risks of anesthesia. The anesthesiologist will discuss these with you.
Updated:
September 16, 2017
Sources:
Surgical repair of an iatrogenic ureteral injury, Up To Date
Reviewed By:
Greenstein, Marc, DO,Sather, Rita, RN