Tricuspid Valve Repair Surgery
Tricuspid Valve Repair Surgery
What is tricuspid valve repair?
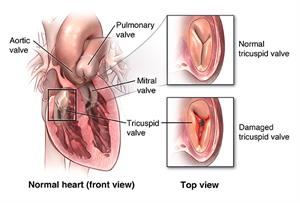
Between the right atrium and the right ventricle is the tricuspid valve. It is 1 of 4 valves in your heart. These valves help manage blood flow through the 4 chambers of your heart. The valves are made of flaps that work together to open and close to keep blood flowing the right direction through the heart.
When the flaps don’t close properly, blood leaks back into a chamber of the heart instead of moving forward. This condition is called tricuspid regurgitation (TR).
When the flaps don’t open enough, blood is forced through too small an opening. This condition is called tricuspid stenosis, which is rare. It typically occurs with other valve abnormalities.
Causes of tricuspid valve problems include birth defects, rheumatic fever, infection, left ventricular heart failure, pulmonary hypertension, and changes that come with aging.
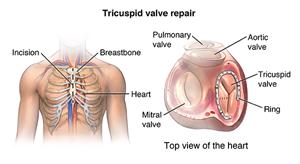
Surgeons can use several techniques to repair a leaking tricuspid valve. These include attaching bands to support the valve, inserting rings around the valve base (annulus), and using specific types of stitches to help the valve flaps work better.
Surgeons may repair the valve with open-heart surgery or laparoscopic surgery.
Why might I need tricuspid valve repair?
You may need tricuspid valve repair if your valve is leaky or can't open properly. You may need surgery to correct a birth defect or damage from endocarditis, an infection of your heart tissue. When the problem is just with the tricuspid valve, successful valve repair could help you regain energy and endurance. However, isolated repair of the tricuspid valve alone is rare. Surgeons usually repair this valve during another planned heart surgery.
What are the risks of tricuspid valve repair?
Tricuspid valve repair is major surgery that requires general anesthesia (you will be put to sleep and will not feel pain during the surgery). Any general anesthesia has the risk of heart or brain injury. Major surgery also carries the risk of blood clots forming during or after surgery. These clots can break free and travel to your lungs (pulmonary embolism), to your brain (stroke), or block blood flow as the clot becomes lodged in other blood vessels.
Other risks of the procedure include:
- Bleeding
- Infection
- Pneumonia
- Damage to nearby organs, tissues, or nerves
- Scarring
- Endocarditis
- Reaction to medication
- Arrhythmia (irregular heartbeats)
- Heart block requiring a pacemaker
- Inability to repair valve requiring valve replacement
- Death
There may be other risks, depending on your specific medical condition. Be sure to discuss any concerns with your doctor before the procedure.
How do I get ready for tricuspid valve repair?
Before tricuspid valve surgery, your doctor will evaluate your medical condition. Your surgeon will use echocardiogram and cardiac catheterization to find out how your tricuspid valve is working and help plan for your surgery. An echocardiogram is an ultrasound of the heart to look at the valve and heart muscle function. Cardiac catheterization is a test done to look at blood flow through the arteries of the heart muscle and to measure the pressure inside of the heart and the lungs.
- Your doctor will explain the procedure and ask if you have any questions.
- You will sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is not clear.
- Your doctor may do a complete physical exam to ensure you are in otherwise good health before undergoing the procedure. You may have blood tests or other diagnostic tests.
- You will be asked to fast for 8 hours before the procedure, generally after midnight.
- You may be asked to shower the night before surgery or the morning of surgery using an antibacterial scrub to prevent infection of the incision sites.
- If you are pregnant or think you could be, tell your doctor.
- Tell your doctor if you are sensitive to or are allergic to any medicines, iodine, latex, tape, or anesthetic agents (local and general).
- Tell your doctor of all medicines (prescription and over-the-counter) and herbal supplements that you are taking.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect blood clotting. You may be told to stop some of these medicines before the procedure.
- Your doctor may request a blood test before the procedure to determine how long it takes your blood to clot.
- Tell your doctor if you have a pacemaker or other implanted cardiac devices.
- If you smoke, stop smoking as soon as possible before the procedure. This may improve your chances for a successful recovery from surgery and benefit your overall health status.
Based on your condition, your doctor may request other specific preparations.
What happens during tricuspid valve repair?
Heart valve repair surgery requires a stay in a hospital. Procedure may vary depending on your condition and your surgeon’s practices. Generally, heart valve repair surgery follows this process:
For open-heart surgery
- You will be asked to remove any jewelry or other objects that may interfere with the procedure.
- You will change into a hospital gown and empty your bladder.
- A healthcare professional will start an intravenous (IV) line in your arm or hand. You may be given IV antibiotics before the procedure starts.
- Additional catheters will be inserted in your neck and wrist to monitor the status of your heart and blood pressure, and to take blood samples. Catheters may also be inserted under the collarbone and the groin.
- The anesthesiologist will monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery. Once you are sedated, a breathing tube will be inserted through your throat into your lungs and you will be connected to a ventilator, which will breathe for you during the surgery.
- A nurse will insert a catheter into your bladder to drain urine.
- Your doctor will insert a transesophageal echocardiogram (TEE) probe into your esophagus to view the valve function after repair.
- A member of the surgical team will clean the skin over the surgical site with an antiseptic solution.
- The doctor will make an incision (cut) down the center of the chest from just below the Adam's apple to just above the navel.
- The doctor will divide the sternum (breastbone) in half lengthwise with a special operating instrument. He or she will separates the two halves of the breastbone and spread them apart to expose the heart.
- To perform this delicate valve repair, your doctor will need to stop the heart. Before stopping the heart, he or she will insert tubes into the heart so that the blood can be pumped through your body by a cardiopulmonary bypass machine.
- Once the blood has been diverted into the heart-lung bypass machine for pumping, your doctor will stop the heart by injecting it with a cold solution.
- When the heart has stopped, the repair will begin. The procedure performed will depend on the type of valve problem you have, for example, separation of fused valve leaflets, repair of torn leaflets, or the reshaping of valve parts so they work better.
- Once the procedure has been completed, your doctor will allow the blood circulating through the bypass machine to re-enter your heart. He or she will shock your heart with small paddles to restart its electrical activity. Gradually, your heart will resume pumping the blood through your body and your doctor will remove the tubes connecting you to the heart-lung machine.
- Once your heart is beating again, the doctor will observe the heart to assess the function of the heart and the valves.
- Your doctor may insert temporary wires for pacing into your heart. These wires can be attached to a pacemaker and your heart can be paced, if needed, during the initial recovery period.
- Your doctor will insert tubes into your chest to drain blood and other fluids from around the heart. These tubes will be connected to a suction device to drain fluids away from the heart.
- Your doctor will rejoin the sternum and sew it together with small wires.
- Your doctor will sew the skin over the sternum back together and close it with sutures or surgical staples.
- A tube will be inserted through your mouth or nose into your stomach to drain stomach fluids.
- A sterile bandage or dressing will be applied.
For a laparoscopic procedure
If your surgeon performs a laparoscopic procedure, he or she will insert special tools into your chest through several smaller incisions, rather than a single large incision. These tools will contain a camera, as well as all the instruments needed to repair your valve. This procedure might take longer than traditional open-heart surgery but recover may be easier.
What happens after tricuspid valve repair?
In the hospital
- After the surgery, a member of the surgical team will take you to the recovery room or the intensive care unit (ICU) to be closely monitored for several days. A nurse will connect you to monitors that will constantly display your electrocardiogram (ECG) tracing, blood pressure, other pressure readings, breathing rate, and your oxygen level. Heart valve repair surgery generally requires a hospital stay of several days or longer.
- You may have a tube in your throat connected to a ventilator (breathing machine) until you are stable enough to breathe on your own. As you wake up from the anesthesia more and start to breathe by yourself, your doctor will adjust the breathing machine to allow you to take over more of the breathing. When you are awake enough to breathe completely by yourself and able to cough, your doctor will remove the breathing tube. He or she may also remove the stomach tube at this time.
- After the breathing tube is out, your nurse will help you cough and take deep breaths every couple of hours. This will be uncomfortable due to soreness, but it is very important that you do this to keep mucus from collecting in your lungs and possibly causing pneumonia.
- Your nurse will give you pain medicine if you are hurting. Ask for the medicine before you become extremely uncomfortable. Your nurse will show you how to hug a pillow tightly against your chest while coughing to help ease the discomfort.
- You may be on special IV drips to help your blood pressure and your heart and to control any problems with bleeding. As your condition stabilizes, your doctor will gradually decrease and then turn off these drips as your condition allows.
- Once the breathing and stomach tubes have been removed and your condition has stabilized, you may start liquids to drink. You can add more solid foods as you can handle them.
- When your doctor determines that you are ready, you will be moved from the ICU to a postsurgical unit or acute care unit. Your recovery will continue to progress. Your activity will be gradually increased as you get out of bed and walk around for longer periods.
- A member of your healthcare team will make arrangements for a follow-up visit with your doctor.
At home
Once your doctors feel that you have recovered enough, you may go home. At home, you must follow all your instructions for medicines, pain control, diet, activity, and wound care. Your doctor might prescribe anticoagulant drugs to help prevent blood clots. Make sure you understand how to take them or how these drugs might affect your health and lifestyle choices. Be sure to keep all your follow-up appointments. Other common instructions after surgery include:
- Walk as much as possible.
- Avoid any heavy lifting. Your doctor will provide a specific timeline.
- Gradually resume normal activities as much as possible (ask your doctor about driving, working, and sexual activity). You will not be able to drive a car for a period after the surgery to allow for healing of the breastbone (sternum) and muscles of the chest wall. Plan to have someone give you a ride home from the hospital.
- Watch your wounds for any sign of swelling, redness, bleeding, or discharge and report these to your medical and surgical team
- Tell your doctor about any increasing pain, fever, chest pain, or shortness of breath.
- Eat a heart-healthy diet and maintain a healthy weight. Eat foods that are low in salt, cholesterol and fat. Try to eat a diet rich in fruits, vegetables and lean meats.
- Don't smoke or use any other tobacco products including electronic cigarettes.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
Updated:
March 22, 2017
Sources:
2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease. Journal of the American College of Cardiology. 2008;52(13):e66-e68., Mild-to-moderate functional tricuspid regurgitation in patients undergoing valve replacement for rheumatic mitral disease: the influence of tricuspid valve repair on clinical and echocardiographic outcomes. Kim, JB. Heart. 2012;98:24-30.
Reviewed By:
Fetterman, Anne, RN, BSN,Mancini, Mary, MD