Pituitary Gland Surgery
Pituitary Gland Surgery
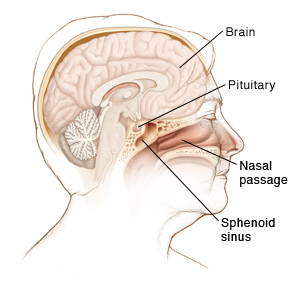
Pituitary gland surgery is done to remove a growth (tumor) that forms in the pituitary gland. This gland is at the base of the brain, behind your nose and sinuses. It makes hormones that control growth, sexual function, and fluid balance. It also controls other glands in your body, such as the thyroid and adrenal glands.
Problems can occur when a tumor forms in the pituitary gland. These tumors are almost always benign (not cancer). But a tumor can cause the pituitary to make too much or too little of some hormones. This can lead to health problems. Or a tumor may press on the nerves to the eyes (optic nerves). This can cause headaches and vision loss.
Surgery to remove the tumor can relieve such problems. In most cases, the surgery is done through the nasal passages. This leaves no scars or stitches that can be seen.
Getting ready for your surgery
Follow any instructions from your healthcare provider.
Tell your provider about any medicines you are taking. You may need to stop taking all or some of these before the surgery. This includes:
All prescription medicines
Over-the-counter medicines such as aspirin or ibuprofen
Street drugs
Herbs, vitamins, and other supplements
Follow any directions from your provider about not eating or drinking before surgery.
The day of surgery
The surgery takes about 3 hours. Before the surgery begins:
An IV (intravenous) line is put into a vein in your arm or hand. You will receive fluids and medicines through the IV.
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine puts you into a state like a deep sleep through the surgery.
Just before the surgery, a breathing tube (endotracheal tube) is placed into your throat through your mouth. The tube is usually removed at the end of surgery or soon afterward.
During surgery
In most cases, surgery is done through the sphenoid sinus. This is one of the air spaces behind the nose. For large or complicated pituitary tumors, a craniotomy is done with the approach through the skull. During trans-sphenoid surgery:
The surgeon may use a surgical microscope to get a close-up view of the gland. In this case, a small cut (incision) is made in your nose or lip. This makes it possible to enter the sphenoid sinus and reach the tumor. Or, a thin tube (endoscope) may be used. This tube has a light and tiny camera on one end. It’s put in through your nostril and into the sphenoid space to reach the tumor.
Once the tumor has been reached, the surgeon will remove it. If the whole tumor can’t be reached, the part that is left may need to be removed during a later surgery. Or it may be treated with radiation. If a large tumor is removed, the area may be filled with a small piece of fat taken from your belly (abdomen).
At the end of surgery, any incisions are closed with stitches. These dissolve on their own in a few weeks. A spongy material (packing) and splints may be placed in your nose.
Recovering in the hospital
You will be taken to a recovery room to wake up from the anesthesia. Right after surgery, you will have a dressing taped to your nose to absorb drainage. You will be given pain medicine. Tell your provider if you are still in pain. You are then taken to a hospital room to stay for 1 to 2 nights. During your stay:
For the first few days or weeks, you will have a stuffy nose and a headache.
You may be given a steroid medicine. (This is not the same as anabolic steroids used by some athletes.) This medicine helps control hormone levels. These levels can change as your body adjusts to your surgery. You will slowly take less and less of the steroid over a week.
For the first day or two after surgery, your urine output will be watched closely. This is to check for a condition called diabetes insipidus. This is a common condition after pituitary gland surgery. It makes you feel thirsty and urinate more than normal. It usually goes away on its own within a week or so.
Recovering at home
Once you are ready to go home, you will be released to an adult family member or friend. Plan to have someone stay with you for the next couple of days to help care for you as your healing begins. Be sure to follow all of your healthcare provider’s instructions. During your recovery:
Take all medicines as directed. This includes pain medicines, steroids, and other medicines you are prescribed. Do not stop taking steroids without talking to your provider first. Steroids should not be stopped suddenly.
Use a salt nasal spray as directed. This keeps the lining of your nose moist and aids healing.
Don't sneeze, cough, or blow your nose for at least 2 weeks after surgery. If you can’t avoid sneezing, keep your mouth open.
Don't bend, lift, or strain for 4 weeks after your surgery.
Go back to your normal activities as advised. Try to do a little more each day.
When to call your healthcare provider
Call your provider if you have any of the following:
Chest pain or trouble breathing (call 911)
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
Symptoms of infection at the incision. These include increased redness or swelling, warmth, more pain, or bad-smelling drainage.
A clear watery drainage from your nose or down the back of your throat
Headaches or other pain not relieved by medicine
Dizziness, stiff neck, or sensitivity to light
Loss of vision or double vision
Constant thirst that is not relieved by drinking
More frequent passing of urine than before surgery
Lightheadedness or fainting
Pain or swelling in your legs
Follow-up
During follow-up visits, your healthcare provider will check on your healing:
If you have packing or splints that need to be removed, this may be done about 7 days after surgery.
If some of the tumor was not removed, you may need more surgery or treatment. You will discuss this with your provider.
About 3 months after your surgery, an eye test and MRI (magnetic resonance imaging) may be done. You will have more imaging tests over time. You will also have blood tests to check your hormone levels. These tests make sure that the tumor has not come back.
Some hormone levels may not return to normal after surgery. If so, you may be given medicines to control or supplement those hormones. Lifelong checking of the gland and your hormone levels is often needed after surgery. Have regular checkups as advised.
Risks and possible complications
All procedures have some risk. Risks of pituitary gland surgery include:
Leaking of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid)
Damage to the pituitary gland
Diabetes insipidus
Infection
Bleeding or blood clot in the brain
Scarring inside the nose
Vision loss
Not able to smell or taste
Injury to blood vessels
Risks of anesthesia
Updated:
September 02, 2017
Sources:
Transsphenoidal surgery for pituitary adenomas and other sellar masses. UpToDate
Reviewed By:
Hurd, Robert, MD,Image reviewed by StayWell medical illustration team.