Understanding Pericardiectomy
Understanding Pericardiectomy
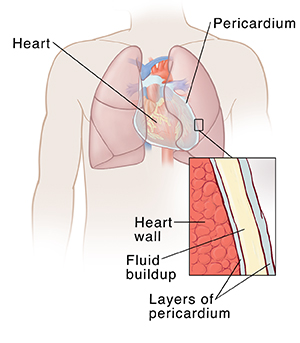
Pericardiectomy is a surgery to remove part or all of the sac around the heart. This lets the heart move more freely.
Why pericardiectomy is done
A fibrous sac surrounds the heart. The sac is called the pericardium. It’s made of 2 thin layers with a small amount of fluid between them. Normally, this sac is thin and flexible. But repeated inflammation can cause it to become stiff and thick. This is called chronic constrictive pericarditis. When this happens, the heart can’t move normally and fill up with as much blood as it should. This can cause increased pressure in the heart, and symptoms such as fatigue and swelling in the body. Cutting the sac away allows the heart to fill normally again. It does not fix the problem that caused the inflammation.
How pericardiectomy is done
Your procedure will be done by a by a cardiothoracic surgeon. This is a doctor who does surgery on the heart. Don’t eat or drink at least 8 hours before the surgery. Your doctor may tell you to stop taking certain medicines before the procedure. You may be asked to shower or bathe with soap or a special cleanser the night before and day of surgery. The surgery can be done in more than one way. In general it goes like this:
You will be taken to the operating room and asked to lay on the operating table on your back. You may be given medicine to relax before being transported.
The anesthesiologist will place a catheter in a vein in your hand to give you fluid and medicine.
You may have additional IV lines placed in your neck. These are to measure the blood pressure in your heart.
You will be given medicine to put you into a deep sleep. A breathing tube will be placed down your windpipe and you will be connected to a breathing machine.
A thin tube will be placed in your bladder to drain urine.
The surgeon will make a large incision down the front of your chest over your breastbone, and cut the bone lengthwise to expose the pericardium. Or the surgeon will make small incisions in your chest to insert the camera and tools.
If the heart-lung machine is needed, an incision will be made in your groin. A blood thinner will be given in your vein by the anesthesiologist, and a tube will be placed in the artery and vein in the groin so that you can be connected to the heart-lung machine. The machine will take over the circulation of the blood in your body while the surgeon is working on the pericardium.
Once the pericardium is removed, if you are on the heart-lung machine, the machine will be gradually turned off and the tubes removed. The incision in your groin will be closed.
Tubes will be left in the chest to drain fluid and blood.
The breast bone will be closed with wires and the skin will be closed with either staples or suture.
You will then be taken to the recovery room or ICU.
Risks of pericardiectomy
All surgery has some risks. The risks of pericardiectomy include:
Not enough oxygen getting out to the body (low cardiac output syndrome)
Excess bleeding
Damage to the heart muscle
Infection
Pneumonia
Fluid buildup around the lungs
Blood clot, which can lead to stroke or other problems
Abnormal heart rhythms (arrhythmias) that can cause death in rare cases
Heart attack
Damage to the blood vessels in the groin
Complications from anesthesia
Death
Your own risks may vary according to your age, your general health, and the reason for your procedure. They may also vary depending on the structure of your heart and pericardium. Talk with your healthcare provider about which risks apply most to you.
Updated:
March 21, 2017
Sources:
Ghavidel A, Gholampour M, Kyavar M. Constrictive pericarditis treated by surgery. Tex Heart Inst J. 2012;39(2):199-205., Hoit BD. Diagnosis and treatment of pericardial effusion. UpToDate., Imazio M. Treatment of acute pericarditis. UpToDate.
Reviewed By:
Fraser, Marianne, MSN, RN,Image reviewed by StayWell medical illustration team.,Mancini, Mary, MD,Pierce-Smith, Daphne, RN, MSN, CCRC