Pelvic Laparoscopy
Pelvic Laparoscopy
A short hospital stay. (You can most likely go home the same day.)
A quick recovery
Minimal anesthesia
Small external scars
Mild to moderate postoperative pain
Getting ready
To prepare for surgery:
Tell your surgeon about any medicines you take. Include herbs, supplements, and over-the-counter medicines. You may need to stop taking certain medicines, such as aspirin, for 7 to 10 days before surgery.
Do not eat or drink anything after the midnight before surgery.
Arrange for a ride home after surgery.
Before the procedure
You will most likely be given general anesthesia to make you sleep during the procedure. A catheter may be inserted to drain urine from the bladder.
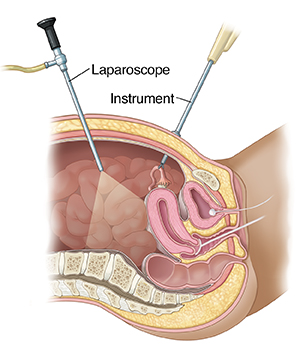
How pelvic laparoscopy is done
One or more small (quarter- or half-inch) incisions are made near the navel or the pubic hairline, or on either side of the lower belly. The laparoscope is inserted through an incision. It sends images to a video screen, allowing the surgeon a close-up view of the organs. Gas is used to inflate the belly, allowing the surgeon room to see and work. Depending on what is found, surgery to treat the problem may be done at this time.
After the procedure
You’ll be taken to a post-op area to wake up and recover from anesthesia.
You may feel some shoulder pain. This is due to irritation from the gas used to inflate the belly.
You may have some discharge from the vagina. If so, ask the nurse for a pad.
You will be asked to walk around to improve breathing and blood flow.
If you had a catheter, it will most likely be removed before you go home.
You can go home as soon as you recover from anesthesia and your condition is stable.
Your recovery
Recovery time depends on which procedure was done through the laparoscope. Your recovery from pelvic laparoscopy may take up to 6 weeks. If it was a simple procedure, like tubal ligation, then 2 weeks is reasonable. For laparoscopic hysterectomies, the recovery may be closer to 6 weeks. While you recover, be sure to follow your healthcare provider’s instructions. During this time:
Take pain medicine as prescribed.
Start eating solid food when you feel ready. To avoid constipation, eat fruits, vegetables, and whole grains. Drink plenty of fluids.
Don’t lift anything heavy until your healthcare provider says it’s safe.
Take it easy for a few days. Ask your healthcare provider when you can return to work, exercise, and sex.
Arrange for a follow-up visit with your healthcare provider to discuss the results of the procedure.
Call your healthcare provider
Contact your healthcare provider right away if you have any of the following:
Have chills, or a fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
Notice that the incision is red, swollen, or draining
Have heavy, bright-red vaginal bleeding or a smelly discharge
Have difficulty urinating
Experience severe belly pain or bloating
Have leg pain, redness, or swelling
Have persistent nausea or vomiting
Are not improving daily
Fainting
Trouble breathing
Updated:
October 07, 2017
Sources:
Abdominal access techniques used in laparoscopic surgery. UpToDate, Guidelines for the Diagnosis, Treatment and Prevention of Postoperative Infections. Larsen J. Infectious Diseases in Obstetrics and Gynecology. 2003;11(1):65-70., Overview of gynecologic laparoscopic surgery and non-umbilical entry sites. UpToDate
Reviewed By:
Freeborn, Donna, PhD, CNM, FNP,Sacks, Daniel, MD, FACOG