Incontinent Urinary Diversion
Incontinent Urinary Diversion
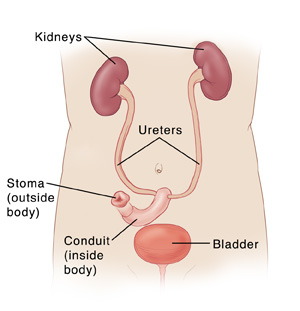
Urinary diversion is surgery that creates a new way for urine to pass out of the body. This may be needed if the bladder is diseased or damaged. Or it may be needed if another problem in the body keeps the bladder from working properly. With incontinent urinary diversion, urine drains through a hole (stoma) in the abdomen into a bag. Here is how the surgery is done.
Changes to your body
After the surgery, urine no longer leaves the body through your urethra. Instead, it drains through a hole made in your lower belly called a stoma. Urine then passes through the stoma and drains into a bag worn outside the body, under your clothes. You’ll need to wear the bag all of the time. And you’ll need to empty and change the bag regularly. You’ll also need to take care of your stoma and the skin around it. You’ll be taught how to do this while you’re in the hospital.
Preparing for surgery
Prepare for the surgery as you’ve been told. In addition:
Tell your doctor about all medicines you take which includes prescription, over-the-counter, herbs and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may be told to stop taking some or all of them before surgery.
Don't eat or drink during the 8 hours before your surgery. This includes coffee, water, gum, and mints. (If you have been instructed to take medicines, take them with a small sip of water.)
If you have been told to, prepare your bowel for surgery (called bowel prep.) This process begins 1 to 2 days before the surgery. Your doctor may tell you to restrict your diet to clear liquids. You may also be asked to take laxatives or to give yourself an enema. Follow all instructions you are given.
The day of surgery
The surgery takes 3 to 4 hours. Afterward, you will stay in the hospital for 5 to 7 nights.
Before the surgery begins:
An intravenous (IV) line is placed in a vein in your arm or hand. This supplies fluids and medicines (such as antibiotics). In some cases, a central or arterial line is inserted into a blood vessel somewhere else on the body. Your doctor can tell you more.
You may get medicine to prevent blood clots in your veins.
You may get a urinary catheter placed in your bladder through your urethra.
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine lets you sleep comfortably through the surgery. A tube may be inserted into your throat to help you breathe.
You may have an epidural to help control post-surgery pain. A small tube is inserted into your back to deliver pain medicine that numbs the lower body. Talk to your doctor or anesthesiologist about this option.
During the surgery:
An incision is made in the lower abdomen.
The bladder may be left in place or it may be removed.
A piece of your small or large intestine (bowel) is then removed. It is used to make a new tube (conduit) for urine to flow from the ureters out of the body. If a piece of small bowel is used, this is called an ileal conduit. If a piece of large bowel is used, this is called a colon conduit.
With either type of conduit, one end is connected to the ureters. The other end is brought through an incision in the abdominal wall to form the stoma.
When the surgery is complete, the incisions are closed with stitches (sutures) or staples.
A small tube (drain) may be placed near the incisions. This drains fluid that may build up after the surgery.
Tubes called stents may be placed through the stoma into the ureters. These help drain urine until healing is complete.
Recovering in the hospital
After the surgery, you will be taken to a recovery room where you will be monitored as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. When you are ready, you will be taken to your hospital room. While in the hospital:
You will be given medicine to manage pain. Let your providers know if your pain is not controlled.
You’ll first receive IV fluids. In a day or so, you’ll start on a liquid diet. You will then slowly return to a normal diet.
As soon as you’re able, you will get up and walk.
You’ll be taught coughing and breathing techniques to help keep your lungs clear and prevent pneumonia.
An ostomy nurse will show you how to care for your stoma and bag.
Drains and stents will likely be removed while you’re in the hospital. If not, you’ll be shown how to care for them at home.
Make sure to get a contact number for your doctor, ostomy nurse, and hospital before you go home. This is in case you have problems or questions after the surgery.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days, to help care for you. Recovery time varies for each person. Your doctor will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Make sure to:
Take all medicines as directed.
Care for your incision as instructed. If you go home with a catheter or drains, take care of them as you were shown.
Care for your stoma as instructed.
Follow your doctor’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incision to be covered with water until your doctor says it’s OK.
Don't lift anything heavy or do strenuous activities, as directed.
Don't drive until your doctor says it’s OK. Don't drive if you’re taking medicine that make you drowsy or sleepy.
Walk a few times daily. As you feel able, slowly increase your pace and distance.
Don't strain to pass stool. If needed, take stool softeners as directed by your doctor.
Drink plenty of water every day. This helps prevent urine odor and dehydration.
When to call your healthcare provider
Call your healthcare provider right away If you have any of the following:
Chest pain or trouble breathing (call 911)
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, worsening pain, or foul-smelling drainage
Pain, redness, swelling, odor, or drainage at the stoma site
Decreased or no urine output for longer than 4 hours
Blood clots in the urine (some pink-tinged urine is normal)
Pain that cannot be controlled with medications
Nausea and vomiting that won’t stop
Pain or swelling in the legs
Follow-up care
You’ll have follow-up visits so your doctor can check how well you’re healing. Sutures, staples, or tubes will be removed. You and your doctor can also discuss any further treatment you may need. If you’re having trouble adjusting to your stoma and bag, talk to your doctor or ostomy nurse. You may also want to consider joining a support group for people with stomas. Ask your nurse for more information.
Risks and possible complications
Bleeding (may require a blood transfusion)
Infection
Blood clots
Pneumonia or other lung problems
Problems with the stoma
Abnormal levels of vitamins or minerals in the blood, requiring lifelong medication
Scarring and narrowing of the ureters
Bowel obstruction
Risks of anesthesia. The anesthesiologist will discuss these with you.
Updated:
September 23, 2017
Reviewed By:
Greenstein, Marc, DO,Sather, Rita, RN