Having Laparoscopic Hernia Repair: TAPP
Having Laparoscopic Hernia Repair: TAPP
What is laparoscopy?
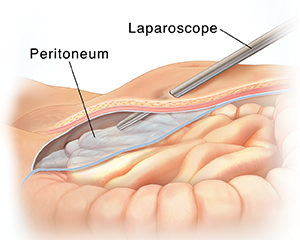
Your hernia operation will be done with a technique called laparoscopy. For this, a thin lighted tube called a laparoscope is used. The scope allows the surgeon to work through a few small incisions. This is instead of the one larger incision that is made for open surgery. Recovery from laparoscopy is often faster and less painful than from open surgery.
What is TAPP?
TAPP is one way to do a hernia repair. It stands for “transabdominal preperitoneal.” The peritoneum is a membrane that covers the organs in the abdomen. During TAPP, the peritoneum is opened to reach the hernia.
Preparing for your surgery
Schedule tests as you have been told. These make sure your heart and lungs are healthy for surgery.
Tell your healthcare provider about all medicine you take. This includes aspirin, NSAIDs, blood thinning medicines (such as warfarin), herbs and other supplements. You may need to stop taking some or all of them before surgery.
Ask your healthcare provider for help to quit smoking. This will help stop the hernia from being strained by smoker’s cough. It will also promote good blood flow for healing.
Avoid heavy lifting. It can strain your hernia and make it worse.
Follow any directions you are given for taking medicines and for not eating or drinking before surgery.
Plan to have an adult family member or friend drive you home from the surgery. Arrange for help with chores and errands while you recover.
During the procedure
The surgery takes 1 to 2 hours. You can likely go home the same day. Before the surgery begins, an IV line is put into a vein in your arm or hand. This line supplies fluids and medicines.
To keep you free of pain during the surgery, you’ll be given anesthesia. This may be general anesthesia. This medicine puts you in a state like deep sleep through the procedure. Or, you may be given regional anesthesia. This numbs the abdomen and makes you relaxed and drowsy through the surgery.
The surgeon makes 2 to 4 small incisions in the abdomen. The scope is put through one of the incisions. The scope sends live pictures to a video screen. This allows the surgeon to see inside the abdomen. Surgical tools are placed through the other small incisions.
Your abdomen is inflated with carbon dioxide. This gas provides space for the surgeon to see and work to repair the hernia.
After the repair, a patch of strong mesh is put over the weak spot in your abdominal wall. The patch acts like a patch on a tire. It stays in place permanently.
The gas is released from your abdomen. Your incisions are then closed with sutures.
For a small number of people, the laparoscopic procedure may not be able to be performed due to certain factors and the surgeon will have to perform an open procedure. These factors can include obesity, past history of abdominal surgery, bleeding, and the inability to see the organs. The surgeon will make this decision either before or during the procedure.
Risks and possible complications of hernia repair
Bleeding
Infection
Numbness or pain in the groin or leg
Urinary retention (inability to urinate)
Bowel or bladder injury
Hernia comes back or new hernia forms
Injury to testes
Problems from mesh
Risks of anesthesia
Updated:
March 21, 2017
Sources:
Abdominal Access Techniques Used in Laparoscopic Surgery. UpToDate., Laparoscopic inguinal hernia repair: transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) approach: a prospective randomized controlled trial. Krishna Asuri. Surgical Endoscopy. 2012;26:639–649.
Reviewed By:
Freeborn, Donna, PhD, CNM, FNP,Lehrer, Jenifer, MD