During Cervical Disk Surgery
During Cervical Disk Surgery
During surgery, your surgeon may remove all or part of the disk (diskectomy). To reach the cervical spine, he or she may make an incision in the front (anterior) or the back (posterior) of your neck. With the anterior approach, the neck may be made more stable with a fusion (joining) of the vertebrae. With the posterior approach, bone may be removed to enable your surgeon to reach the disk.
 Adding stability: fusion
Adding stability: fusion
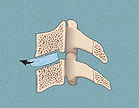
After removing a disk from the front, your surgeon may fuse the vertebrae above and below it. This limits movement, helping to relieve pressure and pain. First, the surgeon enlarges the space between the vertebrae. The surgeon then “plugs” the space with a plastic or metal cage filled with bone chips or stem cells or a cylinder- or wedge-shaped bone graft. Metal plates may be added. As you heal, the graft and vertebrae grow together (fuse). After fusion, your ability to bend your neck may be slightly restricted.
Through the back: posterior approach
Your surgeon will make an incision (about 2 to 4 inches long) in the middle or next to the middle of the back of your neck. Then he or she may remove bone to reach the problem area. The surgeon then removes the damaged portion of the disk.
 Removing bone
Removing bone
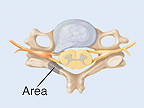
To reach the disk from the back, your surgeon may enlarge the foramina or remove a portion of the lamina. To help relieve pressure on the nerves or spinal cord, bone spurs may also be removed. The location and amount of bone removed depend on the type of problem you have.
 Through the front: anterior approach
Through the front: anterior approach
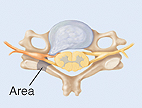
Your surgeon will make a horizontal or vertical incision (about 1 to 3 inches long) on either side of your neck. To reach the disk, soft tissue is moved aside. All or part of the disk that is irritating the nerve is then removed. Your surgeon may remove bone spurs. The vertebrae may then be prepared for a fusion.
Updated:
May 09, 2018
Reviewed By:
Jasmin, Luc, MD,Sather, Rita, RN