Craniotomy
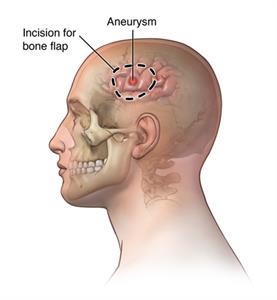
A craniotomy is the surgical removal of part of the bone from the skull to expose the brain for surgery. The surgeon uses special tools to remove the section of bone (the bone flap). After the brain surgery, the surgeon replaces the bone flap and attaches it to the surrounding bone with small titanium plates and screws. If part of the skull bone is removed and not replaced right away, it is called craniectomy. This is done if swelling is likely after brain surgery or if the skull bone flap can't be replaced for other reasons. After a few weeks to months, you may have a follow-up surgery called a cranioplasty. During a cranioplasty, the missing piece of skull will be replaced with your original bone, a metal plate, or a synthetic material.
.
For some craniotomy procedures, doctors use MRI or CT scans. Imaging helps guide the doctor to the exact place in the brain that is to be treated. When computers and imaging are combined to make 3-D pictures, it called image-guided craniotomy or stereotactic craniotomy.
A craniotomy can be done with various tools that help the surgeon see the area of the brain. These include loupes, a microscope, high-definition cameras, or an endoscope. A craniotomy with an endoscope involves putting a lighted scope with a camera into the brain through a small hole in the skull.
Doctors may do a craniotomy for a variety of reasons, including to:
- Diagnose, remove, or treat brain tumors
- Clip or repair an aneurysm
- Remove blood or blood clots from a leaking blood vessel
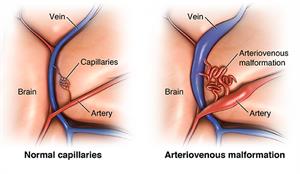
- Remove an arteriovenous malformation (AVM). This is an abnormal mass of blood vessels.
- Drain an infected pus-filled pocket (abscess)
- Repair skull fractures
- Repair a tear in the membrane lining the brain (dura mater)
- Relieve pressure within the brain (intracranial pressure) by removing damaged or swollen areas of the brain that may be caused by traumatic injury or stroke
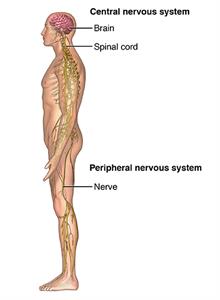
- Treat epilepsy. This is a neurological condition involving the brain that makes people more likely to have seizures.
- Implant stimulator devices to treat movement disorders such as Parkinson disease or a type of movement disorder called dystonia
- Treat hydrocephalus
There may be other reasons for your doctor to recommend a craniotomy.
Any surgery can have complications. Brain surgery risk is tied to the specific place in the brain that the operation will affect. For example, if the area of the brain that controls speech is operated on, then speech may be affected. Some more general complications include:
- Infection
- Bleeding
- Blood clot
- Infection of the lungs (pneumonia)
- Unstable blood pressure
- Seizures
- Muscle weakness
- Brain swelling
- Leakage of the fluid that surrounds and cushions the brain (cerebrospinal fluid)
- Risks of general anesthesia
The following complications are rare and generally relate to specific places in the brain:
- Memory problems
- Speech difficulty
- Paralysis
- Abnormal balance or coordination
- Coma
There may be other risks depending on your specific health condition. Discuss any concerns with your healthcare provider before the procedure.
Check with your healthcare provider about what to do to prepare for the procedure. Below is a list of common steps that you may be asked to do.
- You will be asked to sign a consent form that gives permission to do the surgery. You will need to sign a separate form for getting anesthesia. Read the form carefully and ask questions if something is not clear.
- In addition to a complete health history, your doctor will do a physical exam to make sure you are in otherwise good health before you undergo the surgery. You may also need blood tests and other diagnostic tests.
- You will have a neurological exam before surgery that will be compared with one done after surgery.
- You will be asked to fast before the procedure, generally after midnight.
- If you are pregnant or think you might be, tell your doctor.
- Tell your doctor if you are sensitive to or are allergic to any medicine, latex, tape and anesthetic medicines, either local or general.
- Tell your doctor of all prescribed medicines, over-the-counter medicines, and herbal supplements that you are taking.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any blood-thinning medicine, aspirin, or other medicine that affects blood clotting. You may need to stop these before the procedure.
- If you smoke, you should stop smoking as soon as possible before the procedure to improve your chances for a successful recovery.
- You may be asked to wash your hair with a special antiseptic shampoo the night before the surgery.
- You may get medicine (sedative) before the procedure to help you relax.
- Based on your condition, your doctor may request other specific preparation.
A craniotomy generally requires a hospital stay of 3 to 7 days or more, depending on your condition. You may also go to a rehabilitation unit for several days after your hospital stay. Procedures may vary depending on your condition and your doctor's practices.
Generally, a craniotomy follows this process:
- You will take off any clothing, jewelry, or other objects that may interfere with the procedure and put on a hospital gown.
- An IV (intravenous) line will be put in your arm or hand so you can get fluids and medicines.
- A urinary catheter will be put in to drain your urine.
- You will be placed on the operating table to give the surgeon the best access to the side of the brain to be operated on.
- The anesthesiologist will watch your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- Staff will shave your head and clean the skin over the surgical site with an antiseptic solution.
- The surgeon may use various types of incisions, depending on the affected area of the brain. If an endoscope is used, the incisions may be smaller.
- Your head will be held in place by a Mayfield 3 pin head holder or similar device. The device will be removed at the end of the surgery.
- The surgeon will pull up your scalp and clip it to control bleeding.
- The surgeon may use a medical drill to make burr holes in the skull. He or she may use a special saw to carefully cut the bone.
- The bone flap will be removed and saved.
- The surgeon will separate the thick outer covering of the brain directly underneath the bone (dura mater) from the bone and carefully cut it open to expose the brain.
Extra fluid will be allowed to flow out of the brain, if needed. Your surgeon may use microsurgical instruments, such as a surgical microscope to magnify the area being treated. This gives the surgeon a better view of the brain
In the hospital
Right after the procedure, you will be taken to a recovery room to be closely watched before being taken to the intensive care unit (ICU). In some cases, you may be taken directly to the ICU from the operating room.
In the ICU, you may be given medicine to decrease the brain swelling.
You may have in place a brain intracranial pressure (ICP) device to monitor the pressure in your brain. Or you may have an external ventricular drain (EVD) to remove extra cerebrospinal fluid (CSF). These devices are usually removed after a few days.
You may have various catheters to get or drain fluid, or to monitor your blood pressure.
Your recovery will vary depending on the type of procedure done and the type of anesthesia you had. Once your blood pressure, pulse, and breathing are stable and you are alert, you may be taken to the ICU or your hospital room.
After staying in the ICU and your condition is stable, you will move to a room in the hospital. You will stay in the hospital for several more days.
You may need oxygen for a while after surgery. Generally, the oxygen will be stopped before you go home.
You will be taught deep-breathing exercises to help re-expand the lungs and prevent pneumonia.
Medical staff will check your brain function often and make sure your body systems are working properly after surgery. To check your brain function, you will be asked to follow a variety of basic commands, such as moving your arms and legs. Your pupils will be checked with a flashlight, and you will be asked questions to assess your awareness. These might include your name, the date, and where you are. The staff will test the strength of your arms and legs.
The head of your bed may be raised to prevent swelling of your face and head. Some swelling is normal.
You will be encouraged to move around as you are able while in bed. As your strength improves, you will have help to get out of bed and walk around. A physical therapist (PT) may evaluate your strength, balance, and mobility, and give you suggestions for exercises to do both in the hospital and at home.
You will likely have sequential compression devices (SCDs) placed on your legs while you are in bed to prevent blood clots. SCDs have an air compressor that slowly pumps air into and out of fitted sleeves that are placed on the legs. They help prevent blood clots by passively compressing the leg veins to keep blood moving.
Depending on your case, you may be given liquids to drink a few hours after surgery. Your diet may be gradually changed to include more solid foods, as you can tolerate them.
You may have a catheter in your bladder to drain your urine for a day or so, or until you are able to get out of bed and move around. Be sure to report any painful urination or other urinary symptoms that occur after the catheter is removed, as these may be signs of an infection that can be treated.
Depending on your status, you may be moved to a rehabilitation facility for a period to regain your strength.
Before you are discharged from the hospital, arrangements will be made for a follow-up visit with your doctor. Your healthcare provider will also give you instructions for home care.
At home
Once you are home, it is important to keep the incision clean and dry. Your doctor will give you specific bathing instructions.
You may choose to wear a loose turban or hat over the incision. Do not wear a wig until the incision is completely healed (about 3 to 4 weeks after surgery).
The incision and head may ache, especially with deep breathing, coughing, and exertion. Take a pain reliever for soreness as recommended by your healthcare provider. Aspirin or other blood thinning medicines may increase the chance of bleeding. Be sure to take only recommended medicines and ask if you are unsure.
Continue the breathing exercises used in the hospital to prevent lung infection. You will be advised to avoid exposure to upper respiratory infections (colds and flu) and irritants, such as tobacco smoke, fumes, and environmental pollution.
Gradually increase your physical activity as tolerated. It may take several weeks to return to your previous level of energy and strength.
You may be instructed to not lift heavy items for several weeks to prevent strain on your surgical incision.
Don't drive until your doctor gives you permission.
Seek medical care right away if you have any of these symptoms:
- Fever or chills
- Redness, swelling, bleeding, or drainage from the incision site or face
- Increased pain around the incision site
- Vision changes
- Confusion or excessive sleepiness
- Weakness of your arms or legs
- Speech difficulty
- Difficulty breathing, chest pain, anxiety, or change in mental status
- Green, yellow, or blood-tinged sputum (phlegm)
- Seizure activity
Following a craniotomy, your healthcare provider may give you other instructions about what to do after a craniotomy.
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
Updated:
May 24, 2018
Sources:
Brain Tumor Surgery. American Brain Tumor Association.
Reviewed By:
Jasmin, Luc, MD,Sather, Rita, RN