Cervical Disk Replacement Surgery
Cervical Disk Replacement Surgery
What is cervical disk replacement surgery?
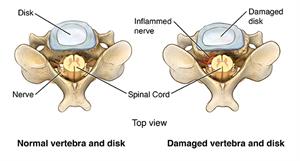
Your cervical spine is made up of the 7 bones, called cervical vertebrae, stacked on top of each other forming the neck area. The cervical disks are the cushions that lie between the cervical vertebrae. They act as shock absorbers to allow your neck to move freely.
Your cervical spine also forms a protective tunnel for the upper part of your spinal cord to pass through. This part of your spinal cord contains the spinal nerves that supply your upper body with sensation and movement. This part also contains all of the nerves coming or going to the lower half of your body.
When the space between your vertebrae becomes too narrow, part of your vertebrae or your cervical disk can press on your spinal cord or spinal nerves, causing you pain, numbness, or weakness. When these symptoms do not respond to nonsurgical types of treatment, disk surgery may be recommended.
Cervical disk replacement surgery involves removing a diseased cervical disk and replacing it with an artificial disk. Before this procedure was available, the affected disk was removed and the vertebrae above and below were fused together to prevent motion
The use of an artificial disk to replace your natural cervical disk is a newer type of treatment. Disk replacement surgery may help preserve movements. It may also help create less stress on the disks above and below compared with cervical fusion surgery.
Disk replacement is not for everyone. Fusion may be better if your spine is not stable, or if your neck has an abnormal curve.
Why is cervical disk replacement surgery needed?
Loss of space between your cervical vertebrae from cervical disk degeneration, or wear and tear, is common. Cervical disks begin to collapse and bulge with age; this happens to most people by age 60. But health care providers don’t know why some people have more symptoms from cervical disk degeneration than others.
Symptoms may include:
- Neck pain
- Neck stiffness
- Headache
- Pain that travels down into your shoulders or into your arms
- Weakness of your shoulders, arms, hands, or legs
- Numbness or "pins and needles" feeling in your arms
What are the risks of cervical disk replacement surgery?
While any surgery carries some risk, disk replacement surgery is a relatively safe procedure. Before you have surgery, you will need to sign a consent form that explains the risks and benefits of the surgery.
Disk replacement is a newer type of spine surgery so there is less information on possible long-term (more than 10 years) risks and outcomes. Discuss with your surgeon the risks and benefits of disk replacement surgery compared with more traditional types of cervical spine surgery.
Some potential risks of cervical spine surgery include:
- Reactions to the anesthesia
- Bleeding
- Infection
- Nerve injury
- Spinal fluid leak
- Voice change
- Stroke
- Difficulty breathing
- Difficulty swallowing
- Failure to relieve symptoms
- Broken or loosened artificial disk
- Need for further surgery
There may be other risks, depending on your specific medical condition. Be sure to discuss any concerns with your surgeon before the procedure.
How do I get ready for cervical disk replacement surgery?
Ask your health care provider to tell you what you should do before your surgery. Below is a list of some common steps that you may be asked to do.
- Tell your surgeon about any medications you take at home including herbal supplements and over-the-counter medications. You may be asked to stop taking aspirin or other medications that thin your blood and may increase bleeding.
- Tell your surgeon if you or someone in your family has any history of reaction to general anesthesia.
- If you smoke, you may be asked to stop smoking well before surgery and avoid smoking for a time after surgery.
- Before surgery you will probably be given instructions on when to stop eating and drinking. It’s common to have nothing to eat or drink after midnight on the night before the procedure.
- Ask your surgeon if you should take your regular medications with a small sip of water on the day of the procedure.
What happens during cervical disk replacement surgery?
Just before the procedure starts you will have an intravenous line (IV) started so you can receive fluids and medications to make you relaxed and sleepy. This procedure is usually done under general anesthesia (you are asleep). Medication may be given through the IV to put you to sleep and a tube may be inserted in your throat to protect your airway and supplement your breathing. The actual procedure may last a few hours. This is what may happen once the procedure begins:
- Monitors are placed to check your heart, blood pressure, and oxygen level.
- The area of your neck where the incision will be made is cleaned with a special solution to kill germs on the skin.
- A one- to two-inch incision (surgical cut) is made on the side or front of your neck.
- The important structures of the neck are carefully moved to the side until the surgeon can see the bones of the vertebrae and the cervical disk.
- The cervical disk that is being replaced is removed.
- The artificial disk is secured into the empty disk space.
- The incision is closed using absorbable sutures (stitches) under the skin. The skin is then carefully closed with sutures that minimize any scarring.
- A small dressing is applied over the incision, a rigid or soft neck collar may be put on your neck to restrict motion, and you will be taken to the recovery area.
Some steps might be slightly different from those outlined above. Talk with your health care provider about what might happen during your procedure.
What happens after cervical disk replacement surgery?
In the recovery area, you will be observed until you recover from the anesthesia. Pain after disk replacement surgery is normal and you may be given pain medication in the recovery area.
Most people will need to spend a day or two in the hospital. This is what may happen during your hospital stay:
- Intravenous fluids may be continued until you can drink fluids well by mouth.
- Once you are able to drink normally, you will be able to start eating your normal diet.
- You’ll continue to take pain medication if you need it.
- Your nurses will check your dressing and help you to get out of bed and go to the bathroom.
- You may be given a support collar to wear in the hospital.
- You will be encouraged to get out of bed and move around as soon as you are able to.
Recovery and rehabilitation at home may be a little different for each person, but in general, here’s what you might expect:
- You may need to continue wearing a soft or rigid neck support.
- You will be able to eat your normal diet.
- You may need to return to your surgeon to have sutures removed.
- You will gradually start returning to normal activities. You should ask your surgeon about any activity restrictions and when you can take a regular shower or bath.
- You may start physical therapy after a few weeks.
- You should be able to return to full activities by 4 to 6 weeks.
You should call your surgeon if you have any of these problems:
- Fever
- Headache
- Bleeding, redness, swelling, or discharge from your incision site
- Pain that does not respond to pain medication
- Numbness or weakness
- Difficulty swallowing
- Voice change or hoarseness
- Difficulty breathing
Your health care team may give you other instructions about what you should do after your procedure.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
Updated:
May 23, 2018
Reviewed By:
Jasmin, Luc, MD,Sather, Rita, RN