Central Line (Central Venous Access Device)
Central Line (Central Venous Access Device)
What a central line does
A central line is often used instead of a standard IV (intravenous) line when you need treatment for longer than a week or so. The line can deliver medicine or nutrition right into your bloodstream. It can also be used to measure blood flow (hemodynamic monitoring), to draw blood, or for other reasons. Ask your healthcare provider why you need the central line and which type you’ll get.
Types of central lines
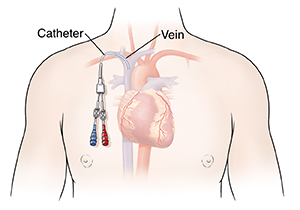
The central line will be placed into 1 of the veins as described below. Which vein is used depends on your needs and overall health. The catheter is threaded through the vein until the tip sits in the large vein near the heart (vena cava). Types of central lines include:
Peripherally inserted central catheter (PICC). This line is placed in a large vein in the upper arm, or near the bend of the elbow.
Subclavian line. This line is placed into the vein that runs behind the collarbone.
Internal jugular line. This line is placed into a large vein in the neck.
Femoral line. This line is placed in a large vein in the groin.
Placing the central line
The central line is placed in your body during a brief procedure. This may be done in your hospital room or an operating room. Your healthcare team can tell you what to expect. During central line placement:
You’re fully covered with a large sterile sheet. Only the spot where the line will be placed is exposed. The skin is cleaned with antiseptic solution. These steps lower the risk for infection.
Medicine (local anesthetic) is injected near the vein. This numbs the skin so you don’t feel pain during the procedure.
After the pain medicine takes effect, the catheter is gently passed into the vein. It’s moved forward until the tip of the catheter is in the vena cava, close to the heart.
The other end of the catheter extends a few inches out from your skin. It may be loosely attached to the skin with stitches to hold it in place.
The healthcare provider flushes the catheter with saline solution to clear it. The solution may include heparin, which prevents blood clots.
An X-ray or other imaging test is done. This allows the provider to confirm the catheter’s position and check for problems.
Risks and complications
As with any procedure, having a central line placed has certain risks. These include:
Infection
Bleeding problems
An irregular heartbeat
Injury to the vein or to lymph ducts near the vein
Inflammation of the vein (phlebitis)
Air bubble in the blood (air embolism). An air embolism can travel through the blood vessels and block the flow of blood to the heart, lungs, brain, or other organs.
Blood clot (thrombus) that can block the flow of blood. A blood clot can also travel through the blood vessels and block the flow of blood to the heart, lungs (pulmonary embolism), brain, or other organs.
Collapsed lung (pneumothorax) or buildup of blood between the lungs and the chest wall (hemothorax)
Nerve injury
Accidental insertion into an artery instead of a vein
Catheter not positioned correctly
If you have any problems with your central line, talk to your healthcare provider.
Updated:
March 13, 2018
Sources:
Rupp, SM. Practice guidelines for central venous access: a report by the American Society of Anesthesiologists Task Forceon Central Venous Access. Anesthesiology (2012); 116(3); pp, 539-573
Reviewed By:
Image reviewed by StayWell medical illustration team.,Mancini, Mary, MD,Ziegler, Olivia, MS, PA