Abdominoplasty (Tummy Tuck)
Abdominoplasty (Tummy Tuck)
Abdominoplasty is often called a “tummy tuck.” During this procedure, excess fat and skin can be removed from your belly. And certain muscles can be repositioned to improve abdominal weakness. Keep in mind that the results will vary for each person. Discuss your treatment goals with your healthcare provider ahead of time. He or she can tell you more about what the surgery can do for you.
Preparing for surgery
Prepare for the surgery as you have been told. In addition:
-
Tell your healthcare provider about any recent health conditions and all medicines you take. This includes herbs and other supplements as well as illegal or illicit drugs. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery.
-
Don't eat or drink during the 8 hours before your surgery, or as directed by your surgeon. This includes coffee, water, gum, and mints. (If you have been instructed to take medicines, take them with a small sip of water.)
The day of surgery
The surgery takes about 2 to 3 hours. You may go home the same day. Or you may stay overnight.
Before the surgery begins
-
An IV line is put into a vein in your arm or hand. This line delivers fluids and medicines.
-
To keep you pain free during surgery, you’re given general anesthesia. This medicine puts you into a deep sleep through the surgery. A tube may be inserted into your throat to help you breathe.
During the surgery
-
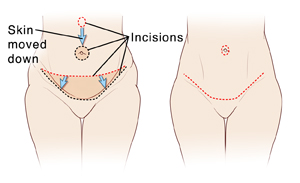
An incision is made in the belly from hipbone to hipbone. This is often along the lower part of the belly just above the pubic hairline. You and your healthcare provider will choose the exact incision site prior to surgery. An incision is also made around the bellybutton.
-
The skin and fat are lifted to expose the abdominal wall beneath. The abdominal wall includes fascia (fibrous tissue) and muscles.
-
If needed, the belly muscles are pulled together to tighten the abdominal wall. Stitches are used down the middle of the belly, to hold the muscles in their new position.
-
After the abdominal wall is tightened, the skin and fat are pulled back down. Excess fat and skin are then removed from the belly.
-
Once the skin and fat are pulled down, the bellybutton may be covered up. In such cases, an incision is made so the bellybutton can be seen. The skin is then sewn into place around the bellybutton.
-
Small tubes (drains) may be placed near the incisions. These drain fluid that may build up as the wound heals.
-
Any incisions made during the surgery are closed with stitches, surgical glue, or both. If stiches are used, they may dissolve on their own. Or they may need to be removed by the healthcare provider at a later date.
After the surgery
You will be taken to a room to wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. You will be given medicines to control pain. If you need to stay overnight, you may be moved to another room. Once you are ready to go home, you will be released to an adult family member or friend.
Recovering at home
Once home, follow any instructions you are given. Your healthcare provider will tell you when you can return to your normal routine. During your recovery:
-
Take any prescribed medicines exactly as directed.
-
Walk slightly bent at the waist, if suggested by your healthcare provider. This helps protect the abdominal wall as it heals.
-
Care for your incisions and the bandage over them as instructed by your healthcare provider.
-
Don’t shower for 72 hours after surgery, or as instructed by your healthcare provider. Don't swim, take a bath, use a hot tub, or do other activities that cause the incisions to be covered with water until your healthcare provider says it’s OK.
-
When you shower, gently wash your incision sites. Then pat the incisions dry. Don’t apply lotions, oils, or creams to the incisions until after they are fully healed.
-
Don’t lift, push, or pull anything heavier than 10 pounds for at least 14 days.
-
Don't do strenuous activity, and exercise as directed. Talk to your healthcare provider about light exercise, such as walking, that you can do to maintain your weight until you’re fully healed.
-
Don’t drive until you are no longer taking prescription pain medicine and your healthcare provider says it’s OK.
-
If advised by your healthcare provider, use a cold pack wrapped in a thin towel to relieve discomfort and control swelling. It’s important not to leave the cold pack on for too long, or your skin could be damaged. Put the pack over your bandages for no more than 20 minutes at a time. Then, leave it off for at least 20 minutes. Repeat this as often as needed during waking hours until swelling starts to improve. Don’t fall asleep with the cold pack on. If you’re not sure how to safely use the cold pack, ask your healthcare provider.
When to call your healthcare provider
Call your healthcare provider if you have any of the following:
-
Chest pain or trouble breathing (call 911)
-
A fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Symptoms of infection at an incision site such as increased redness or swelling, warmth, worsening pain, or foul-smelling drainage
-
Pain that is not relieved by medicine
-
Nothing comes out of your drains for more than 6 hours
-
Pain, swelling, redness, or warmth in your leg, calf, or thigh
Follow-up
You will have follow-up visits so your healthcare provider can see how well you’re healing. If needed, stitches or drains will be removed at one of these visits. To maintain the results of your tummy tuck, take steps to avoid gaining weight. Talk to your healthcare provider if you have questions or concerns.
Risks and complications
Risks and possible complications include:
-
Bleeding
-
Infection
-
Blood clots
-
Excessive scarring
-
Changes in sensation, such as numbness or pain
-
Skin discoloration
-
Death of fat cells deep in the skin (fat necrosis)
-
Damage to nearby nerves, blood vessels, soft tissues, or organs
-
Not being happy with how it looks
-
Risks of anesthesia. Your anesthesiologist will discuss this with you.
Updated:
March 16, 2019
Sources:
Rectus abdominis diastasis. UpToDate
Reviewed By:
Fraser, Marianne, MSN, RN,Lickstein, David, MD