Arsenic poisoning
Arsenic poisoning
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
Activated charcoal, acute promyelocytic leukemia, adenosine triphosphate, AFS, Agency for Toxic Substances and Disease Registry, amebiasis, anemia, arsenic filtration, arsenic poisoning, arsenic trioxide, arsenicosis, arsenobetaine, arsenocholine, atomic florescence spectroscopy, ATP, ATSDR, Ayurvedic medicine, Bangladesh, blackfoot disease, bladder cancer, Bowen's disease, bronchial asthma, cancer, cardiomyopathy, CCA, chicken feed, chromated copper arsenate, chromosomes, copper azole, Department of Agriculture, disodium methyl arsenate, DNA, DSMA, ECG, E. coli, EDTA chelation, electrocardiogram, fish arsenic, folic acid, fossil fuels, glutathione, Gutzeit method, inorganic arsenic, intraepidermal carcinomas, keratosis, kidney cancer, landfill, leukopenia, lung cancer, melanosis, methylated metabolites, monosodium methyl arsenate, MSMA, necrosis, nerve conduction velocity, organic arsenic, peripheral neuropathy, peripheral vascular system, pesticide, polyphenols, propicoazole, psoriasis, radiograph, roxarsone, semiconductors, shallow-tube wells, skin cancer, skin lesions, smelting, squamous cell carcinomas, syphilis, teratogen, toxin, trypanosomiasis, UNESCO, United Nations Educational, Scientific, and Cultural Organization, zinc.
Background
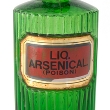
Arsenic is a semi-metallic chemical that occurs naturally in the environment within the earth's crust, in water, and even in smoke from volcanoes. It may be found in soil, water, and human foods, such as chicken. People may become exposed to arsenic by eating or drinking it, breathing it in, and, in rare cases, touching it. People are regularly exposed to arsenic in small doses and can usually metabolize and excrete it without ill-health effects.
However, exposure to too much arsenic may be deadly. Acute poisoning may kill humans quickly, while long-term exposure to certain levels of arsenic may lead to a medical condition called arsenicosis. Arsenicosis may eventually lead to various illnesses (e.g., cancer) or possibly death. Arsenic is a particularly insidious toxin because, depending on its form, it may be odorless, colorless, and flavorless.
Arsenic inhibits essential metabolic enzymes, so it affects many different organs in the body. It leads to the destruction of cells and DNA. Studies have linked prolonged exposure to arsenic with cancer and interrupted fetus development. Other studies have linked arsenic ingestion and exposure to damage to the liver, brain, bladder, lungs, skin, and gastrointestinal system.
Several industries use and produce arsenic. For instance, the wood industry uses the toxin to preserve wood against insects, bacteria, and fungi. Other products that use arsenic or arsenic compounds are electronic devices, such as circuit boards and semiconductors for telecommunications, as well as ammunition and feed for chickens. Farmers primarily used arsenic as a pesticide until the 1940s. It was also used to produce bottles to decolorize glass.
Currently, the United States is the largest importer of arsenic and arsenic compounds in the world. However, as knowledge increases about the ill-health effects of arsenic, its uses have become limited over time.
Arsenic has a long history of medicinal uses, such as treatment for syphilis, psoriasis, and bronchial asthma. In fact, arsenic is still used in medicine. The U.S. Food and Drug Administration (FDA) approved an arsenic compound for one type of leukemia in 2000. Recently published research suggests that traditional Indian medicine, sold over the Internet, uses arsenic in some treatments. Whether medicine producers intended for arsenic to be an ingredient or not is unclear from the study.
The symptoms of acute arsenic exposure may include vomiting, oesophageal and abdominal pain, heart failure, garlic breath, and bloody diarrhea. Health professionals may recognize long-term exposure to low levels of arsenic by looking at the skin. Dark spots (melanosis), thick overgrowths of horny skin (keratosis), and symptoms of skin cancer are the main clues for diagnosis.
The standard treatment for acute arsenic poisoning is chelation therapy with dimercaprol and dimercaptosuccinic acid. Chelation is the administration of agents, usually certain types of chemical compounds that may help the body eliminate arsenic and some other types of metals. These chelating agents may be applied intravenously (injected directly into the bloodstream through the vein) or by using a patch on the skin.
Although folic acid, spirulina, and zinc have been suggested as potential integrative treatments for arsenic poisoning, conclusive evidence of effectiveness is currently lacking.
Because arsenic is widely distributed across the globe in varying quantities and in different states (in water, air, and soil), routinely monitoring people's exposure is important. In areas with high levels of arsenic, prevention, treatment, and education initiatives are necessary.
Technique
General: Arsenic exists in many different states. It may be concentrated in solid rock, dissolved in water, or in the air as a gas. Furthermore, it can exist in a pure elemental state or be combined with other elements to form other compounds.
In 2005, China produced 50% the world's share of arsenic, mostly in the form of arsenic trioxide, a byproduct of gold mining, which is used to treat certain types of cancer. China supplied the United States with 81% of the nation's elemental arsenic from 2001 to 2004, making the U.S. the largest arsenic consumer in the world. The United States imported 11,000 metric tons of arsenic trioxide in 2005 alone.
Arsenic uses:
General: In the United States, arsenic is primarily used to preserve lumber and to make electronic devices, pesticides, and animal feed.
It is also used in some medicines, particularly anticancer medicines.
Lumber: Since the 1940s in the United States, several species of trees have been treated with chromated copper arsenate (CCA), a product made with arsenic that protects the wood from decay and insects.
Prior to 2004, wood preservatives such as CCA accounted for more than 90% the United States' use of arsenic trioxide. Since then, environmentalists concerned about arsenic leaking from the wood into the environment have successfully campaigned for a reduction of CCA treatment.
In 2005, only 65% of arsenic imports were used to make CCA. CCA-treated lumber is now used only for industrial purposes (such as telephone poles) and not residential purposes (such as picnic tables and garden sheds). However, CCA-treated lumber is still widely used in other countries.
Electronic devices: The electronics industry uses a highly pure form of arsenic for equipment such as solar cells, light-emitting diodes, and semi-conductors for telecommunications. Arsenic is also used in space research and microelectronic equipment.
Pesticides: Most pesticides were made from arsenic until the 1940s, when organic pesticides began to replace them. Still, some farmers use less-toxic forms of arsenic to protect their plants from insects, mold, and fungi. Monosodium methyl arsenate (MSMA) and disodium methyl arsenate (DSMA) are the arsenic-based, less-toxic substitutes.
Animal feed: Arsenic is used in some animal feed, particularly chicken feed. Arsenic additives, such as roxarsone, promote chicken growth, improve the pigmentation of meat, and kill parasites. Seventy percent of broiler chickens produced each year in the United States have been fed roxarsone, according to the American Chemical Society. Further spread of arsenic occurs when chicken excrement, which contains arsenic, is used to feed other animals.
Medicine: Arsenic trioxide is a type of antineoplastic drug that has been approved by the U.S. Food and Drug Administration (FDA) for the treatment of promyelocytic leukemia.
In some parts of the world, arsenic is used to treat humans with certain parasitic infections, including trypanosomiasis and amebiasis.
Some veterinarians use arsenic compounds to treat parasites, such as heartworm. However, because arsenic may also have toxic effects, veterinarians often perform blood and serum tests to check the animal's liver and kidney function before treatment.
Some evidence suggests that one-fifth of 193 analyzed Ayurvedic medicines purchased over the Internet contained lead, mercury, or arsenic. Ayurvedic medicine is a system of traditional medicine developed in India.
Arsenic as waste:
General: Although some industries use arsenic, other industries produce it as a waste.
Industries: Electric, gas, and sanitary services are the largest producers of arsenic in the United States, with 1,505,800 total pounds of arsenic released into the environment in 2002, according to Scorecard, a pollution information service. Examples of these companies include Chemical Waste Management of the Northwest, Inc., and one station of Tucson Electric Power.
In 2002, metal industries, such as Sanders Lead Company, released 224,200 pounds of arsenic into the environment. Coal mining operations, such as Patriot Mining Company in Maine, released 57,300 pounds of arsenic, and lumber companies, such as the Langdale Forest Products Company in Georgia, released 500 pounds. Additionally, discarded consumer and industrial electronic equipment released 40 pounds of arsenic into the environment.
California is the largest producer of industrial arsenic waste, followed by Oregon, then Alabama. Industries in some places, such as Sanders Lead Company, Inc., in Alabama and the main plant facility at the Olin Corporation in Illinois, released more than 100 pounds of arsenic into the water in 2002.
Smelting: Metal industries are the largest arsenic polluters of water. This is because arsenic-contaminated wastewater is a byproduct of smelting, an industrial process that separates metals from their ore. Smelting may also produce a gaseous form of arsenic, which may work its way into soil near the smelting equipment. It may be released in the water or the air. Once in the air, it can settle on the ground. Therefore, areas near mining operations may contain a large amount of arsenic. For example, according to a study published in an industrial journal, arsenic was found in high concentrations near gold mines in northern Nevada.
Dumpsites: Some dumpsites, such as some landfills, may be sources of high concentrations of arsenic. For instance, discarded CCA-treated wood and electronic waste may leach arsenic and chemicals into the soil and groundwater.
Arsenic exposure and detection:
General: There are three main ways that people can be exposed to arsenic: ingestion, inhalation, or physical contact. People may be exposed to arsenic as a result of its naturally occurring presence in the environment, or as a result of industrial processes or uses, such as the combustion of fossil fuels.
Ingestion: People ingest arsenic in five primary ways: drinking contaminated water; eating animals whose feed contained arsenic; eating animals that were fed the excrement or parts of animals that had arsenic in their feed; consuming plants that were irrigated with arsenic-contaminated water; and consuming plants that were sprayed with arsenic-based pesticides.
Water: Arsenic in drinking water is a major threat to public health in some areas of the world. Areas near geothermal energy are particularly at risk for high levels. In 2001, the U.S. Environmental Protection Agency (EPA) estimated that 13 million Americans, mostly in western states, are exposed to drinking water that contained more than 0.01 milligrams of arsenic per liter (mg/L) of water. This level is the World Health Organization's (WHO) standard cutoff guideline for safety.
Soil: In West Bengal, a state in Eastern India, and neighboring Bangladesh, arsenic naturally occurs in the soil at high concentrations. Even though the soil is contaminated, the main health risk in this area is from arsenic-contaminated drinking water.
Food: For most of the world, however, the main source of arsenic exposure is through food. Meat, fish, and poultry account for 80% of dietary arsenic intake in the United States, according to the Agency for Toxic Substances and Disease Registry (ATSDR), a division of the U.S. Department of Health and Human Services.
Inhalation: Farmers use pesticides containing arsenic on tobacco plants. As a result, tobacco smokers might inhale small amounts of the toxin.
Inhalation exposure to arsenic may be an occupational hazard for some people. Studies of retired smelters, who are exposed to arsenic gas as they extract metals from their ore, suggest that arsenic particles may remain in the lungs for years. Burning fossil fuels increases arsenic gas levels.
Dermal absorption: Exposure to arsenic through the skin rarely poses a health problem. The only instances of ill-health effects occurring through skin absorption were during industrial accidents, when arsenic compounds were splashed on workers' skin. The WHO considers activities, such as bathing and washing clothes in arsenic-contaminated water, to be safe.
Toxicity: The toxicity, or the harmfulness, of arsenic depends on the type of arsenic, length and concentration of exposure, and the overall health of the person exposed. Gas- and water-based forms tend to be more harmful to humans than solid forms. Inorganic arsenic, or arsenic that is combined with oxygen, chlorine, or sulfur, is usually more toxic than organic arsenic, which is arsenic combined with carbon and hydrogen.
There is evidence that people who are malnourished are more susceptible to poisoning. There is also some evidence that genetics may play a role in how well people can metabolize (break down) and excrete arsenic. Therefore, some people may naturally be more susceptible to poisoning than others.
Mechanism of action: Arsenic is toxic for the body because it impairs the body's ability to produce adenosine triphosphate (ATP), an enzyme in muscle tissue that provides energy for cellular reactions. ATP is necessary for cells of all organisms, and its disruption impacts nearly every system of the body. Arsenic also blocks glutathione, an antioxidant important for detoxification.
Detection in people: Healthcare workers may recognize long-term exposure to low levels of arsenic by looking at the skin. Dark spots (melanosis), thick overgrowths of horny skin (keratosis), and symptoms of skin cancer are the main clues for diagnosis. Various testing procedures can measure arsenic levels in the skin, blood, fingernails, and urine. These tests can determine whether exposure has occurred in the past few days or the past year.
Detection in the environment: Testing arsenic in the environment is difficult, requiring sophisticated techniques, trained staff, and sometimes laboratory evaluation, especially when testing for low levels of arsenic. There are a few laboratory-based analytical methods. One example is called atomic fluorescence spectroscopy (AFS). Laboratory technicians excite arsenic atoms using various forms of radiation. Then they measure the amount of radiation that arsenic emits. These emissions are characteristic of the arsenic, so technicians can identify even small amounts of it. This and other laboratory-based procedures are expensive, require bulky equipment and trained technicians, take a long time to do, and are otherwise difficult to use in field settings.
Field testing: The generally accepted field test for arsenic is inadequate, as well. The Gutzeit method, which has a number of variations, essentially means treating water with a chemical that transforms arsenic in the water into arsine gas. The gas then comes into contact with a paper containing mercuric bromide, a chemical compound that changes color when it is exposed to arsine gas. Analyzing the color of the paper may reveal the concentration of arsenic in the water. Still, the test requires trained technicians to interpret the color, and other compounds (such as selenium) may interfere with the test. Therefore, the test is not considered very accurate or precise.
Scientists are developing new ways to test soil and water that require small and inexpensive equipment and are also time-and labor-efficient.
Arsenic removal and regulation:
General: Once arsenic has been identified in the environment, cleaning, removing, or segregating it depends on what form it takes. Various filters exist to remove the toxin from water. The type of filter that is used depends on the type of water supply and the needs and limitations of the affected community. Removing or encapsulating arsenic-contaminated topsoil is effective but might not be logistically possible if the area is densely populated.
This solution is also very expensive. In 1999, Washington State paid $500,000 to remove 3,086 cubic yards of contaminated topsoil from 10 people's yards, according to secondary sources. Scientists are researching how to chemically stabilize the soil. One example of this procedure, according to some studies, is adding potassium dihydrogen phosphate (KH2PO4). This addition replaces some of the elemental arsenic with phosphate ions. However, this procedure also removes important elements in soil, such as magnesium. More research is necessary before chemically stabilizing arsenic-contaminated soil becomes a safe, effective, and permanent solution.
Regulation: Federal regulations and international guidelines have set standards for how much arsenic is safe.
Drinking water and foods: In drinking water, the EPA set a limit of 0.01 parts per million (ppm) of arsenic in water. The Occupational Safety and Health Administration (OSHA) has also regulated exposure to 10 micrograms of arsenic per cubic meter (μg/m3) in workplace air for full-time employees. The FDA mandates no more than 0.5 parts per million (ppm) of arsenic in uncooked chicken, chicken eggs, and turkey, and two parts per million (ppm) in certain uncooked parts of pigs.
Disposal: There are also federal regulations and international guidelines that address arsenic disposal. The main route of disposal is depositing arsenic-containing materials in a landfill. Wood treated with CCA is not considered hazardous but can only be burned according to state and federal regulations. Arsenic is not usually reclaimed from electronic equipment, but this equipment is still considered hazardous. Arsenic cannot be destroyed in the environment, but can change to less toxic forms.
Theory/Evidence
General: The relationship between arsenic exposure and ill-health effects is not clear. Arsenic exposure is difficult to measure. Ill-health effects that result from long-term, low-level exposure might take years to develop. Therefore, whether arsenic is a direct cause of illness, a contributing cause, or is unrelated is difficult for scientists and medical professionals to determine. The health effects of arsenic are diverse; some, such as diabetes, are not well-substantiated.
Arsenic in food: Also difficult to determine is how hazardous it is to ingest arsenic in food, such as chicken. Arsenic is used in some animal feed, particularly chicken feed. Arsenic additives, such as roxarsone, promote growth, improve the pigmentation of meat, and kill parasites.
Arsenic in chicken: Seventy percent of broiler chickens produced each year in the United States have been fed roxarsone, according to the American Chemical Society. Further spread of arsenic occurs when chicken excrement, which contains arsenic, is used to feed other animals.
However, the amount of arsenic in chicken might not pose a health threat. A report by the Institute for Agriculture and Trade Policy found that neither chicken sold in fast-food restaurants nor in supermarkets exceeded the set safety level (0.5 parts per million). A small sample and a short duration, however, limit the reliability of the research. Furthermore, Americans' consumption of chicken has increased over the past few decades, from 28 pounds per person in 1960 to 87 pounds per person in 2005, according to secondary sources. Despite the increase in chicken consumption, the U.S. Food and Drug Administration (FDA) has not lowered the tolerance level for arsenic in chicken.
Arsenic in fish: Other animals, particularly fish, are exposed to arsenic in the environment. People who eat the fish are, in turn, also exposed. Arsenobetaine and arsenocholine, both also known as "fish arsenic," are minimally dangerous to humans, and are quickly excreted within a few days after ingestion.
Metabolism of arsenic: Low-level exposure to arsenic might have a minimal health impact because the toxin is metabolized (broken down) and excreted through the kidneys. Urinary arsenic is in the form of methylated metabolites that are less toxic than pure, inorganic arsenic. High doses of arsenic impair the body's ability to metabolize arsenic; the body begins to store the toxin in soft tissues instead.
Individual differences: Each person reacts to arsenic differently. For example, any three people similarly exposed to arsenic might develop skin cancer, heart problems, or have no health problems at all. It is unclear why some exposed to arsenic develop arsenicosis and others do not. The factors are as diverse as the symptoms of poisoning. Nutrition, socioeconomic status, and genetics all seem to play a part.
Health professionals, therefore, cannot create a widely accepted definition of arsenicosis (arsenic poisoning). Without a concrete definition, there estimates of how many people experience adverse effects or die from arsenic poisoning are lacking. Furthermore, delayed health effects, poor reporting, and low levels of awareness in arsenic-affected communities make it difficult to provide accurate statistical estimates.
Toxicity case study: West Bengal, a state in western India, and Bangladesh, a country near India, show the interplay of these factors. The World Health Organization (WHO) sets a safety guideline value of 0.01 milligrams of arsenic per liter (mg/L) of water. For much of West Bengal and Bangledesh, groundwater concentrations are five times higher, exceeding 0.05mg/L. More than 92 million people are exposed to water above accepted limits. Although difficult to calculate what the impact of arsenic will be over time, some researchers estimate the arsenic may cause as many as 270,000 cancer-related deaths in Bangladesh annually.
Arsenic contamination: In Bangladesh, people used to collect water from ponds and shallow wells to drink. This method, however, obtained contaminated water that transmitted diseases such as dysentery, typhoid, and hepatitis. To control these diseases, programs initiated in the 1970s dug up to 12 million shallow-tube wells to provide water for almost the entire population. These wells were intended to provide safe drinking water, but had the unforeseen effect of making available arsenic-contaminated water. Digging wells, it turned out, tapped into arsenic that occurs naturally in high concentrations in Bangladeshi soil. The problem expanded when irrigation systems used arsenic-contaminated water for crops, which then, too, become contaminated. The contaminated plants threaten food security and production, according to the United Nations (UN).
Impact on health: Skin lesions are the primary symptoms of arsenic poisoning in West Bengal and Bangladesh in the present day. In 2000, one research group estimated there were 100,000 cases of arsenic-caused skin lesions. The WHO estimates that skin and internal cancers will become the main health concern in the future.
Compounding factors: Poor nutrition, which is more common among people living in poverty, may exacerbate the ill-health effects of arsenic poisoning. Much of West Bengal and Bangladesh is poor, so the effects of contaminated water are expected to be severe. Furthermore, costs of healthcare might be more than poor communities can afford. Communication in this area of the world is more difficult because communication channels are slower, and health officials might lack sufficient knowledge to educate the public about how to keep safe. If people with arsenicosis become too sick to engage in productive activities, the disease can spark a vicious cycle of poverty leading to poor health, thus reinforcing poverty.
Tackling the problem: Government and non-governmental organizations have been tackling the problem of arsenic poisoning in West Bengal and Bangladesh. Water testing and control, digging deeper wells, harvesting rainwater, filtering pond water, treating contaminated water with chemicals, and piping in water from outside sources are all solutions under consideration. According to secondary sources, workers have distributed 30,000 filtration units that will bring water to 400,000 people.
Health Impact/Safety
General: The relationship between arsenic exposure and ill-health effects is not clear. Arsenic exposure is difficult to measure. Ill-health effects that result from long-term, low-level exposure might take years to develop. Therefore, whether arsenic was a direct cause of illness, a contributing cause, or is unrelated is difficult for scientists and medical professionals to determine. The health effects of arsenic are diverse; some, such as diabetes, are not well substantiated.
People respond to arsenic differently. For example, there is evidence that people who are malnourished are more susceptible to poisoning. Some people can metabolize (break down) arsenic better than others, possibly due to a difference in genetic makeup.
Types of Exposure:
General: The toxicity, or the harmfulness, of arsenic depends not only on the person exposed, but also on the form of arsenic. Arsenic exists in many different states; it can be concentrated in solid rock, dissolved in water, or in the air as a gas. Gas- and water-based forms tend to be more harmful to humans than solid forms. Furthermore, it can exist in a pure elemental state, or be combined with other elements to form other compounds. Each compound can have a differing level of toxicity to people and animals. Inorganic arsenic, or arsenic that is combined with oxygen, chlorine, or sulfur, is usually more toxic than organic arsenic, which is arsenic combined with carbon and hydrogen.
Acute exposure: Acute exposure, or exposure to high amounts of arsenic over a short period of time, is rare. However, when it does occur, acute exposure affects the gastrointestinal system, causing nausea, vomiting, diarrhea, and abdominal pain. Acute exposure is also associated with hepatic necrosis, or the death of liver cells, and kidney failure. Acute exposure might cause a heart disorder called cardiomyopathy. Once arsenic leaves the body, whether naturally or using treatments, these symptoms may lessen, as long as exposure caused no permanent damage.
Chronic exposure: Chronic, long-term exposure leading to poisoning, also called arsenicosis, might take 5-10 years to manifest itself, and it affects many systems in the body. It can take the form of a number of ailments.
Inhaled arsenic: Arsenic in different forms can impact the environment and human health differently. Lumber treated with chromated copper arsenate (CCA), an arsenic-based agent designed to protect the wood from pests, may leach into soil and groundwater. If the wood is burned, people may inhale arsenic, which causes changes to the skin, such as dark spots (melanosis) and thick overgrowths of horny skin (keratosis). It may also cause respiratory system cancer and, in rare cases, tumors in the liver, skin, and digestive tract. Arsine gas, found mostly in industrial settings, attaches to red cells after inhalation, and may irreversibly damage cell membranes and kill red blood cells.
Ingested arsenic: People ingest arsenic in five primary ways: drinking contaminated water; eating animals that ate arsenic; eating animals that were fed the excrement or parts of animals that ate arsenic; eating plants that were watered with arsenic-contaminated water; and eating plants that were sprayed with arsenic-based pesticides. The Agency for Toxic Substances and Disease Registry (ATSDR) reports that people chronically exposed to arsenic by ingesting it are particularly vulnerable to skin cancer, and tumors in the bladder, lungs, and sometimes the liver, kidney, and prostate. The World Health Organization (WHO) reports that ingested arsenic also affects the gastrointestinal system.
Ingesting arsenic at high levels, if it does not cause death, may cause nausea, vomiting, abnormal heart rhythm, decreased production of red and white blood cells, and abnormal "pins-and-needles" sensations in the hands and in feet, as well as damage blood vessels.
Signs and Symptoms:
Skin contact with arsenic: The skin does not readily absorb arsenic. The WHO recognizes no health risk from bathing, hand-washing, and washing laundry in arsenic-contaminated water. An area of Everett, a town in Washington State, had high levels of arsenic in the soil because it was near a lead smelter. Smelters extract metals from their ore and create arsine gas as a waste product. Town officials advised residents in this area to wear gloves while gardening and to vacuum their houses daily.
Cancer: Arsenic is a carcinogen, meaning it causes cancer, and seems to cause cancer in many different organs. However, the WHO reports exposure must occur for at least 10 years before cancer develops. Drinking contaminated water may cause skin, lung, bladder, and kidney cancers. Inhaling arsenic can cause lung cancer. The mechanism by which arsenic causes cancer is thought to be through chromosomal damage, or damage to DNA.
However, certain types of arsenic may be used to treat diseases, including cancer. For instance, arsenic trioxide is a type of antineoplastic drug that has been approved by the U.S. Food and Drug Administration (FDA) for the treatment of promyelocytic leukemia.
In some parts of the world, arsenic is used to treat humans with certain parasitic infections, including trypanosomiasis and amebiasis.
Some veterinarians use arsenic to treat parasites, such as heartworm.
Gastrointestinal disorders: Arsenic causes the blood vessels in the gastrointestinal tract to become more permeable, leading to fluid loss. It may kill cells in the wall of the stomach, leading to holes (ulcers). Inflammation and hemorrhaging can cause bloody diarrhea.
Heart disorders: Arsenicosis may cause the heart to beat irregularly. After many years of chronic exposure, problems occur in the peripheral vascular system (i.e., in the hands and feet). Gangrene is a complication of necrosis (i.e., cell death of body tissues). Gangrene causes limbs or extremities to die and rot on the body; amputation may be medically necessary. Gangrene in the extremities (i.e., hands and feet) is called blackfoot disease, and there is some evidence that long-term exposure to arsenic, along with poor nutrition, may cause this malady.
Neurologic disorders: Long-term exposure to arsenic in children may be associated with lower IQ scores, according to the Agency for Toxic Substances and Disease Registry (ATSDR). Peripheral neuropathy, or neurological effects in the hands, legs, and feet, may cause people to feel pain, weakness, numbness, pins-and-needles sensations, or to become paralyzed in these areas. Some evidence exists that hearing loss, epilepsy, and intellectual disability might also occur, according to the ATSDR. Upon removal of arsenic, some people may partially recover from its effects.
Skin disorders: When people are exposed to more than 0.02 milligrams of arsenic per kilogram of body weight per day (kg/day), usually in drinking water, patchy dark spots may occur, usually on eyelids, temples, neck, nipples, and groin. Thickening of the skin into elevations that look like corns is especially likely to occur on the hands and soles of feet. Arsenicosis is believed to cause various forms of skin cancer, including squamous cell carcinomas and intraepidermal carcinomas (Bowen's disease). The prevalence of skin cancer increases with the amount of exposure to arsenic.
Respiratory system disorders: Chronically inhaling high concentrations of arsenic compounds may irritate the cells that line the respiratory system, eventually causing cancer.
Bone marrow disorders: Thrombocytopenia, leukopenia, and anemia (i.e., platelet, white blood cell, and red blood cell deficiencies, respectively) may result from chronic arsenic poisoning.
Reproductive system disorders: Arsenic is a teratogen, which means it interferes with embryonic development. It can transfer across the placenta from the mother to the fetus. As a result, it may kill or deform the developing fetus or baby soon after birth.
Evidence suggests that the amount of arsenic excreted in breast milk is not significant, even in areas where maternal exposure to arsenic is high.
Diagnosis:
General: Characteristic symptoms and medical tests can help health workers identify arsenic.
The identifying symptoms of acute arsenic exposure are vomiting, oesophageal and abdominal pain, heart failure, garlic odor on the breath, and bloody diarrhea. Health professionals may recognize long-term exposure to low levels of arsenic by looking at the skin. Dark spots (melanosis), thick overgrowths of horny skin (keratosis), and symptoms of skin cancer are the main clues for diagnosis. Living near smelters, working in certain industries, and being exposed to pesticides might also help healthcare professionals identify arsenicosis.
Medical tests: Laboratory tests can confirm arsenic exposure. Urine, hair, nails, liver function, and nerve conduction velocity tests, as well as electrocardiogram (ECG), chest radiograph, and a neurologic consultation are some ways that arsenic exposure can be confirmed. An ECG can detect abnormal heartbeats; a radiograph produces an X-ray image of the chest and can show the presence of some types of arsenic compounds. Hair and nail samples can be tested for arsenic levels. Normal urine samples yield arsenic concentrations of less than 50 micrograms of arsenic per liter (µg/L); values above 200 µg/L are considered abnormally high.
Prevention:
General: Knowing whether arsenic exists in dangerously high concentrations in the air, water, and soil helps prevent exposure and illness.
Treated wood: CCA-treated wood should be excluded from firewood piles and home projects.
Drinking water: Drinking water that contains concentrations of arsenic higher than 0.01 mg of arsenic per liter of water (mg/L) should be replaced by clean water for cooking and drinking. Also, deeper wells are often less likely to be contaminated. Rainwater harvesting might be an option for some areas, particularly for those in which deeper wells are not a logistical possibility.
Diet: A balanced diet and good nutrition may be important for preventing and mitigating the effects of arsenic. Plants treated with organic pesticides and animal products that are labeled as antibiotic-free are likely to have lower levels of arsenic than plants treated with arsenic and animals that were fed arsenic. Arsenic is used in chicken feed in part to kill parasites, and is considered an antibiotic. Scientists, however, have not yet proven whether this organic and pesticide-free food has any health benefit over standard foods.
Treatment:
General: Treatment for arsenic poisoning depends on whether exposure is acute or chronic, and what the symptoms are.
Acute exposure: Following exposure to high levels of arsenic, health professionals generally check the patient's heart and breathing. Then healthcare workers usually check to see if the patient is safe from further exposure, wash exposed skin and eyes, and finally stabilize liver function. Fluid replacement and blood transfusions might be necessary for patients who are vomiting or bleeding internally. The Agency for Toxic Substances and Disease Registry (ATSDR) recommends one gram per kilogram of body weight of activated charcoal within one hour of arsenic ingestion, although the effectiveness of this procedure has not been substantiated. If a radiograph confirms the presence of arsenic in the lower gastrointestinal tract, this area should be flushed.
EDTA chelation became well-known during the 1950s, when it was proposed as a method to cleanse the blood and blood vessel walls of toxins and minerals. EDTA, or ethylenediamine tetra-acetic acid, is a synthetic amino acid. For many years, chelation therapy has been used with calcium disodium EDTA to treat heavy metal toxicity. Chelating agents are administered using a dermal patch or intravenously. Chelation therapy may also be used to treat arsenic poisoning, as well as lead, iron, mercury, and cobalt poisoning. However, some research results on the effectiveness of chelation in treating high arsenic levels in the body are mixed. More studies are needed to clarify the therapy's effectiveness. Chelation may be most useful when administered soon after arsenic exposure, slowing its spread throughout the body. The ATSDR recommends 3-5 mg/kg of body weight of the chelating agent dimercaprol every 4-12 hours until symptoms resolve.
Patients taking anticoagulants (drugs, such as heparin, that thin the blood) or antiplatelets (drugs, such as aspirin, that prevent platelets from clumping together) should avoid chelation. People receiving root canal therapy and people who are pregnant or breastfeeding should also avoid chelation.
Chronic exposure: Currently, specific treatment options for chronic arsenic poisoning are lacking. Once the cause of poisoning as been identified, future exposure should be avoided. Treatment may focus on improving the signs and symptoms. It may take several weeks or months after exposure is discontinued for symptoms to resolve. Some symptoms, particularly those that affect the nervous system may be long-lasting or permanent.
Although several integrative therapies have been suggested as potential treatments for arsenic poisoning, evidence of effectiveness is currently lacking.
Folate and folic acid are forms of a water-soluble B vitamin. Folate occurs naturally in food, and folic acid is the synthetic form of this vitamin. Early evidence suggests that folate may lower blood arsenic concentration and thereby contribute to the prevention of arsenic poisoning. Additional research is needed in this area.
People who are allergic or hypersensitive to folate or any folate product ingredients should not use this treatment. People receiving coronary stents or those with anemia or seizure disorders should use this treatment cautiously. It is recommended that pregnant women consume 400 micrograms of folate daily in order to reduce the risk of fetal defects. Folate is likely safe if breastfeeding.
The term spirulina refers to a large number of cyanobacteria or blue-green algae. Spirulina extract plus zinc may be useful for the treatment of arsenic poisoning. However, additional research is needed to confirm early findings.
People who are allergic or hypersensitive to spirulina or blue-green algae should avoid this treatment, and use the treatment cautiously if they have phenylketonuria, autoimmune diseases, bleeding disorders, diabetes, or osteoporosis, or if taking products containing the blue-green algae species Anabaena spp., Aphanizomenon spp., and Microcystis spp. Patients should also use this treatment cautiously if they are underweight, taking anti-obesity agents, appetite suppressants, or if consuming a high-protein diet. This treatment if not recommended for children and pregnant or breastfeeding women
Zinc is generally considered safe when taken at the recommended dosages. Zinc chloride is considered unsafe because evidence of safety and effectiveness are currently lacking. People with kidney disease should not take zinc, and people who are pregnant or breastfeeding should take zinc cautiously.
Selenium is a mineral found in soil, water, and some foods. Selenium has been proposed as a potential treatment for arsenic poisoning. Human and animal studies suggest that selenium helps the body excrete arsenic, reduces arsenic's impact on cells, and prevents arsenic from harming chromosomes. More research is necessary to confirm these effects.
Patients should avoid taking selenium if they are allergic or sensitive to products containing selenium, and/or if they have a history of non-melanoma skin cancer. Selenium is generally regarded as safe for pregnant or breastfeeding women. However, animal research reports that large doses of selenium may lead to birth defects.
Polyphenols: A recent study has shown that black and green tea extracts reduced arsenic-induced damage to DNA in white blood cells that fight infections. Arsenic produces reactive oxygen; polyphenols increased activity of antioxidant enzymes. More research is necessary before the benefits of tea extracts for arsenic poisoning are confirmed.
Future Research or Applications
General: Exposure to arsenic is almost unavoidable for humans. Much of the arsenic that humans are exposed to has little effect and is excreted without incident. However, in the future, health professionals, community members, and educators will focus on new ways to prevent arsenicosis (arsenic poisoning) for everyone all over the world, as well as to mitigate arsenic's effects on the body.
Developing countries: The most concerning and pressing arsenic-related medical issues may be preventing and treating poisoning among severely affected communities in developing countries.
Prevention: Sometimes only small procedural changes can protect communities from arsenic poisoning. For example, arsenic-contaminated water is safe to use for laundry and bathing, but only clean water will suffice for drinking and cooking. Therefore, some communities only need to mark water sources that are clean and contaminated. This may maximize the use of filters that produce arsenic-free water.
Another example of a simple preventative technique is raising rice beds about 15 centimeters above ground, according to the United Nations (UN). This protects the plants from arsenic-contaminated irrigation water.
Communication: Adequate communication can bring about these small, life-saving changes. Educating local health officials and politicians as to how to keep community members safe can help prevent further poisoning.
Reducing contamination: Digging deeper wells can, in some cases, bypass layers of arsenic in the soil, providing cleaner water. Harvesting rainwater runs a risk of breeding mosquitoes, but can also be an option for some communities. Filtering pond water and piping in water from outside sources are all possible solutions. According to secondary sources, by 2007, workers had distributed 30,000 inexpensive filtration units, bringing water to 400,000 people in Bangladesh.
New technology: New technology for identifying levels of arsenic in the environment and arsenic removal from water and soil is emerging.
Modifiedbacteria: Microbial biologists at the University of Edinburgh have genetically modified E. coli, a strain of bacteria, to detect very small amounts of arsenic in drinking water, according to secondary sources. When the modified E. coli comes into contact with arsenic, a gene in the bacteria turns on, and the bacteria will begin to break down lactic acid. By testing the acidity of the arsenic and E. coli contaminated water, untrained workers can easily determine whether arsenic is present. This test requires further investigation in real-world settings, but may be superior to current tests because it is less expensive, more accurate, requires little equipment, and does not require trained professionals to administer the test.
Soilremoval: Scientists are researching how to chemically stabilize arsenic-contaminated soil. One example of this procedure, according to some studies, is adding potassium dihydrogen phosphate (KH2PO4). Although this process can replace some arsenic with phosphate ions, it can also remove important soil elements, such as magnesium. More research is necessary before chemically stabilizing arsenic-contaminated soil becomes a safe, effective, and permanent solution.
Filters: The United Nations Educational, Scientific, and Cultural Organization (UNESCO) has developed filters that use iron-oxide coated sand to absorb arsenic from water. Groundwater treatment plants produce this sand as a waste product. Because it recycles the material, the filter is cost-efficient. Twenty people can use one filter. A filter innovation by the U.S. National Science Foundation and the U.S. Environmental Protection Agency (EPA) is nanofibers that contain a synthetic, aluminum-based compound. Because this filter can be used at water sources, such as pumps and wells, it is convenient.
Developed countries: Developed countries, such as the United States, still struggle to minimize the presence of arsenic in people and the environment. A 2004 Department of Agriculture study suggested a review of "safe" levels of overall ingested arsenic intake. Arsenic in chicken and increased chicken consumption spurred this recommendation.
Poultry industry: Some chicken producers, such as Tyson Foods, have already stopped adding arsenic to chicken feed. Increased public attention to this issue, combined with better government regulations, may help people understand the health risks of eating arsenic-contaminated chicken, and if necessary, reduce the amount of arsenic in food.
Lumber industry: Lumber companies are decreasing the amount of wood treated with chromated copper arsenate (CCA), an arsenic-based compound. They have already ceased using CCA-treated wood for residential purposes, such as picnic tables. Lumber companies may continue to decrease the use of this compound for wood used industrially, substituting it with less hazardous chemicals, such as propicoazole and copper azole.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com)
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Agency for Toxic Substances and Disease Registry. www.atsdr.cdc.gov.
Brammer H, Ravenscroft P. Arsenic in groundwater: a threat to sustainable agriculture in South and South-east Asia. Environ Int. 2009 Apr;35(3):647-54. View Abstract
Das NK, Sengupta SR. Arsenicosis: diagnosis and treatment. Indian J Dermatol Venereol Leprol. 2008 Nov-Dec;74(6):571-81. View Abstract
Environmental Protection Agency (EPA). www.epa.gov.
Gamble MV, Liu X, Slavkovich V, et al. Folic acid supplementation lowers blood arsenic. Am J Clin Nutr. 2007 Oct;86(4):1202-1209. View Abstract
Ghosh P, Roy C, Das NK, et al. Epidemiology and prevention of chronic arsenicosis: an Indian perspective. Indian J Dermatol Venereol Leprol. 2008 Nov-Dec;74(6):582-93. View Abstract
Lorenzen JK, Nielsen S, Holst JJ, et al. Effect of dairy calcium on supplementary calcium intake on postprandial fat metabolism, appetite, and subsequent energy intake. Am J Clin Nutr. 2007 Mar;85(3):678-87. View Abstract
Misbahuddin M, Islam AZ, Khandker S, et al. Efficacy of spirulina extract plus zinc in patients of chronic arsenic poisoning: a randomized placebo-controlled study. Clin Toxicol (Phila). 2006;44(2):135-141. View Abstract
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Saper RB, Phillips RS, Sehgal A, et al. Lead, mercury, and arsenic in US- and Indian-manufactured Ayurvedic medicines sold via the Internet. JAMA. 2008 Aug 27;300(8):915-23. View Abstract
Scorecard: the Pollution Information Site. http://scorecard.org. Accessed May 15, 2009
Sinha D, Dey S, Bhattacharya RK, et al. In vitro mitigation of arsenic toxicity by tea polyphenols in human lymphocytes. J Environ Pathol Toxicol Oncol. 2007;26(3):207-20. View Abstract
World Health Organization (WHO). www.who.int/en.
Zeng H, Uthus EO, Combs GF Jr. Mechanistic aspects of the interaction between selenium and arsenic. J Inorg Biochem. 2005 Jun;99(6):1269-74. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017