Your Child's Hypoplastic Left Heart Syndrome
Your Child's Hypoplastic Left Heart Syndrome
Your child has a hypoplastic left ventricle. This means that the left ventricle is either too small or absent. The most common heart problem that includes a hypoplastic left ventricle is called hypoplastic left heart syndrome (HLHS). This sheet explains HLHS.
In a normal heart, oxygen-poor blood is pumped to the lungs from the right ventricle. Oxygen-rich blood is pumped to the body from the left ventricle. |
With HLHS, oxygen-rich blood can’t be pumped to the body in the normal way because of problems with left-sided heart structures. |
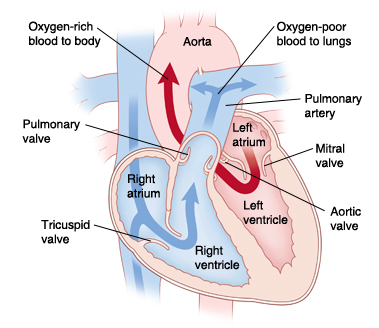
The normal heart
The heart is divided into 4 chambers. The 2 upper chambers are called atria. The 2 lower chambers are called ventricles. The heart has 4 valves. The valves open and close. They keep blood flowing forward through the heart and lungs.
In a normal heart, oxygen-poor blood returning from the body fills the right atrium. This blood flows across the tricuspid valve into the right ventricle. The right ventricle pumps this blood across the pulmonary valve through the pulmonary artery to the lungs. There, the blood receives oxygen. Oxygen-rich blood returns from the lungs and fills the left atrium. This blood then flows into the left ventricle. The left ventricle pumps this blood across the aortic valve to the aorta. From there, it travels out to the body.
The ductus arteriosus is a normal part of a baby’s heart before birth. It’s a blood vessel that connects the pulmonary artery and the aorta. It lets blood flow between the 2 vessels. It normally closes shortly after birth. If it remains open, it’s called a patent ductus arteriosus (PDA).
The foramen ovale is also a normal structure in a baby’s heart before birth. It’s an opening in the wall (atrial septum) between the atria. It normally closes a few weeks after birth. If it remains open, it’s called a patent foramen ovale (PFO).
What is hypoplastic left heart syndrome?
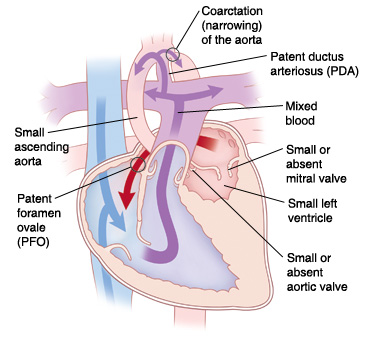
With HLHS, the left side of the heart didn’t develop properly. The left heart structures (mitrial valve, left ventricle, aortic valve, and aorta) are too small or absent. This includes the left ventricle. There may also be narrowing (coarctation) of the aorta.
Because the left ventricle is too small, it can’t do its job. This means that oxygen-rich blood can’t be pumped to the body in the normal way.
Normally after birth, the PFO and PDA close. But, in hypoplastic left heart syndrome, they remain open and allow blood to flow through the heart and reach the body:
The PFO allows oxygen-rich blood from the left atrium to flow through the atrial septum and mix with oxygen-poor blood in the right atrium. This causes mixed blood (blood with some oxygen) to flow into the right ventricle and be pumped through the pulmonary artery.
The PDA allows some of the mixed blood in the pulmonary artery to flow into the aorta. This carries some oxygen to the body. Because the blood contains less oxygen than normal, your child’s skin, lips, and nails may look blue. This is called cyanosis.
If the ductus arteriosus closes after birth, the heart can’t use this path to send oxygenated blood to the body. This causes the child’s organs to fail. At the same time, the lungs become filled with too much blood and fluid. This leads to a problem called congestive heart failure (CHF).
What causes hypoplastic left heart syndrome?
HLHS is a congenital heart defect. This means your child was born with it. The exact cause is unknown. Most cases seem to occur by chance. Having a family member with a left-sided heart problem can make HLHS more likely.
What are the symptoms of hypoplastic left heart syndrome?
A child with HLHS develops severe symptoms shortly after birth. Symptoms can include:
Trouble breathing or rapid breathing
Poor feeding
Tiredness
Irritability
Cyanosis
Enlarged liver
Circulatory collapse (child becomes gray, cold, and the heart may stop beating)
How is hypoplastic left heart syndrome diagnosed?
Your healthcare provider may find HLHS during fetal echocardiography (fetal ultrasound) before your child is born. This test uses sound waves to form a picture of the baby’s heart. This test can be done when you are at least 16 weeks pregnant.
If HLHS isn’t seen before birth, signs may be found during a physical exam shortly after birth.
If your doctor suspects a heart problem, he or she will refer your child to a pediatric cardiologist. This is a doctor who diagnoses and treats heart problems in children. To confirm a diagnosis of HLHS, several tests may be done. These include:
Chest X-ray. X-rays are used to take a picture of the heart and lungs.
Electrocardiography (ECG or EKG). The electrical activity of the heart is recorded.
Echocardiography (echo). Sound waves are used to create a picture of the heart and look for structural defects and other problems.
How is hypoplastic left heart syndrome treated?
HLHS is treated with surgery. This can involve either a series of 3 heart surgeries or, less commonly, heart transplantation. Both treatment options have risks and benefits. Your child’s cardiologist and surgeon will discuss them with you.
In some instances, a hybrid procedure involving a combination of surgery and cardiac catheterization may be used to treat your child in place of the first in a series of 3 surgeries. Your child's cardiologist and surgeon will discuss the risks and benefits of this option with you.
Newborns are given IV medicine to keep the ductus arteriosus open immediately after birth. This lets oxygenated blood reach the body.
Your child may need a procedure called a balloon septostomy soon after birth, if the PFO is too small and there is not sufficient blood flow. This may be done to help until a complete repair can be done. During this procedure, a catheter (thin, flexible tube) with a balloon on the end is used. It is guided through a blood vessel into the heart. The balloon is inflated to widen the PFO. Sometimes, a stent may be placed to keep the hole open. This allows more blood to mix freely between the atria. More oxygenated blood can then reach the body.
What are the long-term concerns?
HLHS continues to be one of the hardest heart problems to treat. After surgery, your child may have ongoing heart problems. Your child may need medicines to manage symptoms and improve heart function. Your child will need more surgery. In the long term, your child may need a heart transplant. In any case, your child will need regular follow-up visits with the cardiologist for the rest of his or her life.
In many cases, children with HLHS can be active. How active will vary with each child. Ask the cardiologist what activities your child can do safely.
Your child may need to take antibiotics before having any surgery or dental work. This is to prevent infection of the heart or valves. This is called infective endocarditis. The cardiologist will give you instructions for this.
Updated:
August 17, 2018
Sources:
Hypoplastic Left Heart Syndrome, Up To Date
Reviewed By:
Ayden, Scott, MD,Bass, Pat F. III, MD, MPH,Image reviewed by StayWell medical illustration team.