When Your Child Needs Bladder Reconstruction Surgery
When Your Child Needs Bladder Reconstruction Surgery
Why is bladder reconstruction surgery needed?
Your healthcare provider recommends surgery to repair your child’s bladder because it isn’t working correctly. During the surgery, the bladder may be patched or rebuilt. In some cases, a new opening (stoma) is made for urine to travel out of the body.
How should we prepare for this surgery?
Tell the surgeon about any medicines your child takes. Include herbs, supplements, and over-the-counter medicines. You may need to have your child stop taking certain medicines, such as ibuprofen, before the surgery.
Discuss with the surgeon any allergies and health problems your child has.
Follow any directions your child is given for not eating or drinking before surgery. This includes any directions for bowel prep. If you do not follow the instructions, the surgery may have to be postponed.
Meet with the child’s anesthesiologist before the surgery. He or she gives your child medicine so your child sleeps and does not feel pain during the surgery. The anesthesiologist also monitors your child’s heart rate, blood pressure, and oxygen levels during the procedure.
What happens before the surgery?
Your child will be given a mild sedative to help him or her relax. When it’s time for the procedure, your child will be given general anesthesia (medicine to help him or her sleep through the surgery). A soft plastic tube (catheter) may be put into the bladder to drain urine during and after surgery.
What happens during the surgery?
One or more of the following may be done:
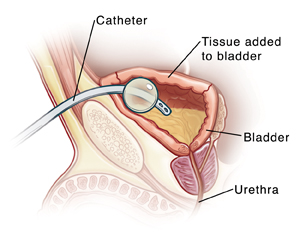
The bladder may be made larger (augmented). This can be done with tissue from another part of the body.
The new bladder can drain through the urethra (tube that carries urine out of the body). Or the new bladder may be drained through a stoma made in the belly (abdomen). A stoma is a new opening for urine to leave the body. To drain urine, a catheter can be inserted into the stoma and removed each time the bladder needs to be emptied.
What happens after the surgery?
You will be able to see your child soon after surgery. Nurses will care for and monitor your child as he or she recovers. Upon awakening, your child may cry and act confused. Medicine will be given to ease any pain. The catheter that was put in place during the surgery will stay in place for about 3 weeks. You will be given detailed care instructions for the catheter.
Recovering from the surgery
Your child may need to stay in the hospital for 4 to 10 days. The healthcare provider will tell you when your child is ready to leave the hospital. If your child had a stoma placed, a healthcare provider will teach you how the stoma is used and how to care for it. As your child heals, the stoma will be checked for problems.
Follow-up care
Before your child leaves the hospital, you will be given instructions for giving care at home. Follow these carefully. Make a follow-up appointment with your child’s healthcare provider within the next 1 to 2 weeks. Your child’s recovery and future care will be discussed during the appointment.
When to call your child's healthcare provider
Unless advised otherwise by your child’s healthcare provider, call the provider right away if:
Your child is of any age and has repeated fevers above 104°F (40°C).
Your child is younger than 2 years of age and a fever of 100.4°F (38°C) continues for more than 1 day.
Your child is 2 years old or older and a fever of 100.4°F (38°C) continues for more than 3 days.
Also call your child’s healthcare provider if your otherwise healthy child has any of the following:
Chills
An incision site or sites that are red, swollen, draining, or bleeding
A tube that is not draining or falls out
Severe abdominal pain or bloating
Nausea or vomiting
Refusal to eat
Pain that doesn’t get better or gets worse
Trouble with the stoma
Tips for helping your child prepare
Many hospitals have staff trained in helping children cope with their hospital experience. This person is often a child life specialist. Ask your child’s healthcare provider for more information about this service. There are also things you can do to help your child prepare for the procedure. The best way to do this depends on your child’s needs. Start with the tips below:
Use brief and simple terms to describe the procedure to your child and why it’s being done. Younger children tend to have a short attention span, so do this shortly before the surgery. Older children can be given more time to understand the procedure in advance.
Make sure your child understands which body parts will be involved in the procedure.
As best you can, describe how receiving anesthesia will feel. For instance, the medicine may be given as gas that comes out of a mask. The gas may smell like bubble gum or another flavor. It will make your child sleepy so he or she naps during the procedure.
Tell your child what he or she will likely see in the operating room during the surgery. For instance, you could mention who will be there or that the person giving your child medicine to help your child nap will be in uniform.
Allow your child to ask questions and answer these questions truthfully. Your child may feel nervous or afraid. He or she may even cry. Let your child know that you’ll be nearby during the procedure.
Use play, if appropriate. With younger children, this can involve role-playing with a child’s favorite toy or object. With older children, it may help to read books about what happens during the procedure.
Updated:
March 20, 2017
Sources:
Merck Manual 2013
Reviewed By:
Adler, Liora, C., MD,Bass, Pat F., III, MD, MPH