When Your Child Needs a Spinal Tap
When Your Child Needs a Spinal Tap
A spinal tap (lumbar puncture) is a test that removes and checks a sample of cerebrospinal fluid (CSF). This fluid surrounds the brain and spinal cord. During the test, a small sample of CSF is removed from the spinal canal. The sample is then studied in a lab. A spinal tap is safe and does not damage the spinal cord or nerves. Within a few hours your child’s body will make new fluid to replace what is removed. From start to finish, the test usually takes about 10 to 15 minutes. 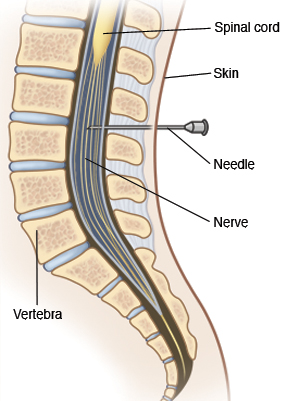
Before the test
Follow all instructions given by your child’s healthcare provider to prepare your child for the test.
Your child needs to lie still during the test. If this will be hard for your child, he or she may be given medicine (a sedative) ahead of time. This will help your child to stay calm during the test. Anesthesia is also an option. This is medicine that makes your child fall asleep and not feel pain during the test. Babies will need to be held in position by staff during the test.
If anesthesia will be used during the test, you’ll be given certain food, drink, and instructions for medicine to prepare your child. For instance, your child may be told to not eat or drink for a certain number of hours before the test.
Let the healthcare provider know
For your child’s safety and best results, tell the healthcare provider if your child:
Takes any prescription or over-the-counter medicines. This includes any medicines that may make your child more likely to bleed, such as aspirin or ibuprofen.
Is allergic to any medicines or iodine.
Has any health problems, including conditions that may raise the risk for bleeding or increased intracranial pressure.
During the test
A spinal tap is done by a trained healthcare provider. Ask your child’s healthcare provider in advance if you can stay with your child in the hospital room. Your child may bring along a favorite toy, such as a stuffed animal, for comfort.
Your child changes into a hospital gown and lies on a hospital bed.
If needed, anesthesia is given to your child. A trained nurse (anesthetist) or specialized healthcare provider (anesthesiologist) helps with this process. Special equipment is then used to watch your child’s breathing, heart rate, and blood pressure.
If your child is awake during the test, he or she is asked to curl into a tight ball and then stay still.
Your child’s lower back is cleansed so that the skin area is sterile.
Medicine is used to numb the area.
A hollow needle is then inserted through the back into the small space that holds the fluid in the spinal canal. Sometimes the needle is inserted more than once to find the best place to draw the fluid. Once the needle is in place, the fluid sample is slowly collected. The pressure of the fluid may also be measured.
After the fluid is collected, the needle is removed. The area is then cleaned and bandaged.
After the test
Your child may be asked to lie still or rest for a few hours after the test. Follow any activity restrictions as advised by your child’s healthcare provider.
Some soreness in the low back is normal. A pain reliever, such as acetaminophen, may be recommended to help manage any discomfort.
Schedule a follow-up appointment with your child’s healthcare provider to review the results of the test.
When to call your healthcare provider
Contact your healthcare provider if your child has any of the following:
Fever (see Fever and children, below)
A seizure caused by fever
Your baby is fussy or cries and can't be soothed
A headache that is severe or lasts longer than 2 days
Muscle aches or lower back pain that is severe or lasts longer than 2 days
Leg tingling or weakness
Any change in behavior or activity level
Your child is confused or hard to wake up
Constant bleeding or clear fluid leaking from the needle site
Your child begins to act sicker or get worse
Fever and children
Always use a digital thermometer to check your child’s temperature. Never use a mercury thermometer. For infants and toddlers, be sure to use a rectal thermometer correctly. A rectal thermometer may accidentally poke a hole in (perforate) the rectum. It may also pass on germs from the stool. Always follow the product maker’s directions for proper use. If you don’t feel comfortable taking a rectal temperature, use another method. When you talk to your child’s healthcare provider, tell him or her which method you used to take your child’s temperature.
Here are guidelines for fever temperature. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Infant under 3 months old:
Ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead temperature of 100.4°F (38°C) or higher, or as directed by the healthcare provider.
Armpit temperature of 99°F (37.2°C) or higher, or as directed by the healthcare provider.
Child age 3 to 36 months:
Rectal, forehead, or ear temperature of 102°F (38.9°C) or higher, or as directed by the healthcare provider.
Armpit temperature of 101°F (38.3°C) or higher, or as directed by the healthcare provider.
Child of any age:
Repeated temperature of 104°F (40°C) or higher, or as directed by the healthcare provider.
Fever that lasts more than 24 hours in a child under 2 years old. Or a fever that lasts for 3 days in a child 2 years or older.
Helping your child get ready
Many hospitals have people trained to help children cope with their medical care or hospital experience. These people are often called child life specialists. Check with your child’s healthcare provider if child life programs or other similar services are available for your child. There are also things you can do to help your child get ready for a test or procedure. How best to do this depends on your child’s needs. Start with the tips below:
Use short and simple words to describe the test to your child. Tell them why it’s being done. Younger children tend to have a short attention span. So talk with them shortly before the test. Older children can be given more time to understand the test in advance.
Tell your child what to expect in the hospital during the test. For instance, you could talk about who will be doing the test and what the hospital room will look like.
Make sure your child understands which body parts will be involved in the test.
As best you can, describe how the test will feel. For instance, if your child is awake during the test, he or she may feel some mild pain or pressure when the needle is inserted. Let your child know that this mild pain won’t last long.
Let your child ask questions and answer these questions truthfully. Your child may feel nervous or afraid. He or she may even cry. Let your child know that you’ll be nearby during the test.
Use play when telling your child about the test, if appropriate. With younger children, this can mean role-playing with a child’s favorite toy or object. With older children, it may help to read books or show pictures of what happens during the test.
Updated:
July 11, 2018
Sources:
Lumbar puncture: Indications, contraindications, technique, and complications in children, UpToDate
Reviewed By:
Bass, Pat F. III, MD, MPH,Jasmin, Luc, MD