When Your Child Has Swimmer’s Ear
When Your Child Has “Swimmer’s Ear” 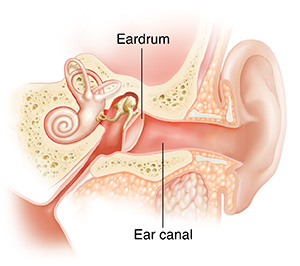
If your child spends a lot of time in the water and is having ear pain, he or she may have developed swimmer's ear (otitis externa). It is a skin infection that happens in the ear canal, between the opening of the ear and the eardrum. When the ear canal becomes too moist, bacteria can grow. This causes pain, swelling, and redness in the ear canal.
Who is at risk for swimmer’s ear?
Children are more likely to get swimmer’s ear if they:
Swim or lie down in a bathtub or hot tub
Clean their ear canals roughly. This causes tiny cuts or scratches that easily get infected.
Have ear canals that are naturally narrow
Have excess earwax that traps fluid in the ear canal
What are the symptoms of swimmer’s ear?
The most common symptoms of swimmer’s ear are:
Ear pain, especially when pulling on the earlobe or when chewing
Redness or swelling in the ear canal or near the ear
Itching in the ear
Drainage from the ear
Feeling like water is in the ear
Fever
Problems hearing
How is swimmer’s ear diagnosed?
The healthcare provider will examine your child. He or she will also ask questions to help rule out other causes of ear pain. The healthcare provider will look for:
Redness and swelling in the ear canal
Drainage from the ear canal
Pain when moving the earlobe
How is swimmer’s ear treated?
To treat your child’s ear, the healthcare provider may recommend:
Medicines such as antibiotic ear drops or a pain reliever that is put in the ear. Antibiotic medicine taken by mouth (orally) is not recommended.
Over-the-counter pain relievers such as acetaminophen and ibuprofen. Don't give ibuprofen to infants younger than 6 months of age or to children who are dehydrated or constantly vomiting. Don’t give your child aspirin to relieve a fever. Using aspirin to treat a fever in children could cause a serious condition called Reye syndrome.
How can you prevent swimmer’s ear?
Ask your child's healthcare provider about using the following to help prevent swimmer’s ear:
After your child has been in the water, have your child tilt his or her head to each side to help any water drain out. You can also dry his or her ear canal using a blow dryer. Use a low air and cool setting. Hold the dryer at least 12 inches from your child’s head. Wave the dryer slowly back and forth—don’t hold it still. You may also gently pull the earlobe down and slightly backward to allow the air to reach the ear canal.
Use a tissue to gently draw water out of the ear. Your child’s healthcare provider can show you how.
Use over-the-counter ear drops if the healthcare provider suggests this. These help dry out the inside of your child’s ear. Smaller children may need to lie down on a couch or bed for a short time to keep the drops inside the ear canal.
Gently clean your child’s ear canal. Don't use cotton swabs.
When to call your child’s healthcare provider
Call your child's healthcare provider if your child has any of the following:
Increased pain redness, or swelling of the outer ear
Ear pain, redness, or swelling that does not go away with treatment
Fever (see Fever and children, below)
Fever and children
Always use a digital thermometer to check your child’s temperature. Never use a mercury thermometer.
For infants and toddlers, be sure to use a rectal thermometer correctly. A rectal thermometer may accidentally poke a hole in (perforate) the rectum. It may also pass on germs from the stool. Always follow the product maker’s directions for proper use. If you don’t feel comfortable taking a rectal temperature, use another method. When you talk to your child’s healthcare provider, tell him or her which method you used to take your child’s temperature.
Here are guidelines for fever temperature. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Infant under 3 months old:
Ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead (temporal artery) temperature of 100.4°F (38°C) or higher, or as directed by the provider
Armpit temperature of 99°F (37.2°C) or higher, or as directed by the provider
Child age 3 to 36 months:
Rectal, forehead (temporal artery), or ear temperature of 102°F (38.9°C) or higher, or as directed by the provider
Armpit temperature of 101°F (38.3°C) or higher, or as directed by the provider
Child of any age:
Repeated temperature of 104°F (40°C) or higher, or as directed by the provider
Fever that lasts more than 24 hours in a child under 2 years old. Or a fever that lasts for 3 days in a child 2 years or older.
Updated:
August 10, 2018
Reviewed By:
Bass, Pat F III, MD, MPH,Image reviewed by StayWell medical illustration team.,Kacker, Ashutosh, MD,Turley, Ray, BSN, MSN