When Your Child Has Non-Hodgkin Lymphoma
When Your Child Has Non-Hodgkin Lymphoma
Your child has been diagnosed with non-Hodgkin lymphoma (NHL). You are likely feeling shocked and scared. You are not alone. Support and treatment are available. Your child’s healthcare team will help you as you make important decisions about your child’s health.
What is NHL?
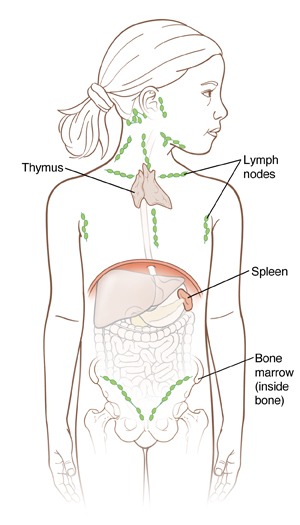
NHL is cancer of the lymphatic system. The lymphatic system is part of the immune system, which helps the body fight infection. The lymphatic system includes:
-
Lymph. Infection-fighting fluid containing a certain type of white blood cell called lymphocytes.
-
Lymph nodes. Small bean-shaped organs that filter lymph and store white blood cells. Lymph nodes are grouped together throughout the body. Some areas where they are found include the neck, armpit, and groin. The lymph nodes may sometimes swell when you have a cold or infection or rarely, when cancer is growing in the lymph node.
-
Bone marrow. Soft spongy tissue found in the center of bones. Blood cells are made in the bone marrow.
-
Thymus. A gland that helps build the immune system in young children. It produces a type of white blood cell called T-lymphocytes, which fight infection. The thymus is located underneath the breastbone.
-
Spleen. Organ that stores certain lymphocytes and filters the blood. It’s located under the ribs on the left side of the body.
-
Other organs in the body, such as the tonsils and digestive tract. These also contain lymphatic tissue.
With NHL, cancer cells form in the lymphatic system. Lymphocytes begin to grow out of control. When the cancerous lymphocytes group together in a lymph node or organ, such as the spleen, they form a tumor. The tumor can spread, or metastasize, to another part of the body, such as the lungs. The cancer cells make it hard for the body to fight infection. The cells can also cause other health problems.
Who gets NHL?
Children at any age can get NHL. But kids between the ages of 10 to 19 are affected most often. NHL affects boys more often than girls. NHL is not contagious. This means your child can’t pass it to another person.
What causes NHL?
With NHL, white blood cells called lymphocytes start to grow abnormally. If the cells come together in lymph nodes or other areas of the body, they can cause tumors to form. What causes this to happen is not fully known. Changes in certain genes, called mutations, may affect the way your child’s cells grow. This gene mutation is often random and couldn’t have been prevented. In rare cases, other factors, such as exposure to certain viruses, chemicals, or radiation, may play a role. But most often, the cause of cancer in children is unknown.
What are the symptoms of NHL?
Some common symptoms of non-Hodgkin lymphoma include fever, night sweats, and swollen lymph nodes in the neck, chest, armpits, or groin.
Other symptoms can depend on the location of the lymphoma:
-
If the lymphoma starts in the belly or abdomen, the child might have belly pain, fever, constipation, and loss of appetite. This is because the tumor is pressing on the organs in this area.
-
If the lymphoma starts in the chest, the child might have trouble breathing, pain with deep breaths, coughing, or wheezing. Lymphomas in the chest can also press on a main blood vessel called the superior vena cava. This can cause swelling and a bluish color in the head and arms. If left unchecked, it can also affect the brain and may even be life-threatening.
Your child may have experienced some of these symptoms, or other symptoms.
What tests are done once NHL is diagnosed?
Your child has had a biospy (removal of a piece of the abnormal area) to diagnose NHL. He or she may also have one or more of the following to learn more about the lymphoma:
-
Blood tests to take a blood sample and test it.
-
Imaging tests to take detailed images of areas inside the body. These may include a chest X-ray, magnetic resonance imaging (MRI), computed tomography(CT) scan, ultrasound, and positron emission tomography (PET) scan.
-
Bone marrow aspirations and biopsies to take samples of bone marrow from the hip bones.
-
Lumbar puncture, also called spinal tap, to take a sample of the fluid around the spinal cord from the child’s lower back.
Staging is the process that determines the size of the cancer and how much it has spread. Your child's healthcare provider uses exams and tests to find out the size of the cancer and where it is. He or she can also see if the cancer has grown into nearby areas, and if has spread to other parts of your body. Staging helps the healthcare team plan treatment for your child. The staging process used for NHL looks at all of the following:
-
Location of the primary tumor
-
If the cancer is all above or below the diaphragm. This is the breathing muscle that separates the chest from the abdomen (belly)
-
If the cancer has spread to other parts of the body
The St. Jude staging system is most commonly used for NHL in children. (A different system is used for NHL in adults.) The cancer is grouped into stages. The stages are written as Roman numerals and can have a value of I through IV (1 through 4). The higher the number, the more advanced the cancer is. For instance, stage I is a very early stage of cancer that's only in one place. Stage IV means the cancer is widespread and found in the brain or spinal cord and/or in the bone marrow.
There are many different types of childhood NHL. Your child’s healthcare provider will talk with you about the type your child has and the stage.
How is NHL treated?
The treatment your child receives depends on the type of NHL he or she has, as well as its stage. Treatments may be combined. Your child may require one or more of the following treatments:
-
Surgery to remove all or part of a tumor. This is not a common treatment for childhood NHL.
-
Chemotherapy, called chemo, or other medicines to kill the cancer cells. Your child may get a combination of medicines. They are given through a small tube, called an IV that’s usually put into a vein in the arm or chest. Or, they may be given by mouth or injection.
-
Radiation therapy to destroy cancer cells and shrink a tumor using strong X-rays. Radiation may be used before or after other treatments.
-
High-dose chemotherapy with a stem cell transplant. Young blood cells, called stem cells, are taken from the child or from someone else. This is followed by a high dose of chemotherapy medicine, and possibly radiation. This causes damage to the bone marrow. After the high-dose chemotherapy, the stem cells are replaced.
Supportive treatments
Supportive treatments help to protect the child from infection, prevent discomfort, and bring the body’s blood counts back to a healthy range. During your child’s treatment, he or she may be given antibiotics. These are medicines that help prevent and fight infection. Other medicines may also be given. These help ease side effects caused by treatment, such as nausea. Your child may also get a blood transfusion to restore the blood cells destroyed by treatment. For a blood tranfusion, blood is taken from a donor and stored until the child is ready to get it.
What are the long-term concerns?
With early treatment, NHL is usually curable. But chemotherapy and radiation may cause some problems, such as damage to certain organs. So your child’s health will need to be watched closely for life. This may include clinic visits, blood tests, imaging tests, and ultrasounds of the heart.
Coping
Receiving a cancer diagnosis for your child is scary and confusing. Remember that you are not alone. Your child’s healthcare team will work with you and your child throughout your child’s illness and care. You may also want to seek information and support for yourself. Learning about your child's cancer and talking with others who also have a child with cancer may help you and your family cope with the changes the cancer brings. Some helpful resources include:
-
Children's Oncology Groupwww.childrensoncologygroup.org
-
Lymphoma Research Foundationwww.lymphoma.org
-
The Leukemia & Lymphoma Societywww.lls.org
Updated:
March 15, 2019
Reviewed By:
Levy, Adam S, MD,Stump-Sutliff, Kim, RN, MSN, AOCNS