When Your Child Has Mouth Sores
When Your Child Has Mouth Sores
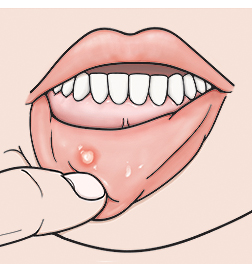
Your child has a mouth sore. Mouth sores can be painful and can make eating or drinking uncomfortable. But they are usually not a serious problem. Most mouth sores can easily be managed and treated at home.
What causes mouth sores?
An injury to the mouth
Certain viruses and illnesses
Stress
Certain medicines
What are the symptoms of mouth sores?
Canker sores are the most common type of mouth sore. They are usually white with red borders. Other types of mouth sores can be white, red, or yellow. Your child may have a single sore or more than one at the same time. Mouth sore symptoms can include:
|
|
NOTE: If your child has a sore outside the mouth, it’s likely a cold sore. Cold sores can be spread through direct contact. They may require different treatment from mouth sores. Ask your child’s healthcare provider for more information about cold sores if you think your child has one.
How are mouth sores diagnosed?
A mouth sore is diagnosed by how it looks. To get more information, the healthcare provider will ask about your child’s symptoms and health history. He or she will also examine your child. You will be told if any tests are needed.
How are mouth sores treated?
Mouth sores generally go away within 7 to 14 days with no treatment.
You can do the following at home to relieve your child’s symptoms:
Give your child over-the-counter (OTC) medicines, such as ibuprofen or acetaminophen, to treat pain and fever. Do not give ibuprofen to infants 6 months of age or less or to a child who is dehydrated or constantly vomiting. Do not give aspirin to a child. This can put your child at risk of a serious illness called Reye’s syndrome.
Cold liquids, ice, or frozen juice bars may help soothe mouth pain. Avoid giving your child spicy or acidic foods.
Liquid antacid 4 times a day may help relieve the pain. For children older than age 6, a teaspoon (5 mL) as a mouthwash may be given after meals. Younger children should have the antacid applied to the mouth sore using a cotton swab.
Use the following treatments only if your child is over the age of 4:
Apply a small amount of OTC numbing gel to mouth sores to relieve pain. The gel can cause a brief sting when applied.
Have your child rinse his or her mouth with saltwater or with baking soda and warm water, then spit. The mouth rinse should not be swallowed.
Call the healthcare provider if your child has any of the following:
A mouth sore that doesn’t go away within 14 days
Increased mouth pain
Trouble swallowing
Signs of infection around a mouth sore (pus, drainage, or swelling)
Signs of dehydration (very dark or little urine, excessive thirst, dry mouth, dizziness)
Fever (see Fever and children, below)
Your child has had a seizure caused by the fever
Fever and children
Always use a digital thermometer to check your child’s temperature. Never use a mercury thermometer.
For infants and toddlers, be sure to use a rectal thermometer correctly. A rectal thermometer may accidentally poke a hole in (perforate) the rectum. It may also pass on germs from the stool. Always follow the product maker’s directions for proper use. If you don’t feel comfortable taking a rectal temperature, use another method. When you talk to your child’s healthcare provider, tell him or her which method you used to take your child’s temperature.
Here are guidelines for fever temperature. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Infant under 3 months old:
Ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead (temporal artery) temperature of 100.4°F (38°C) or higher, or as directed by the provider
Armpit temperature of 99°F (37.2°C) or higher, or as directed by the provider
Child age 3 to 36 months:
Rectal, forehead, or ear temperature of 102°F (38.9°C) or higher, or as directed by the provider
Armpit (axillary) temperature of 101°F (38.3°C) or higher, or as directed by the provider
Child of any age:
Repeated temperature of 104°F (40°C) or higher, or as directed by the provider
Fever that lasts more than 24 hours in a child under 2 years old. Or a fever that lasts for 3 days in a child 2 years or older.
Updated:
February 09, 2018
Reviewed By:
Adler, Liora C., MD,Dozier, Tennille, RN, BSN, RDMS,Turley, Ray, BSN, MSN