When Your Child Has Leukemia
When Your Child Has Leukemia
Since your child has been diagnosed with leukemia, you're likely feeling shocked and scared. But, support and treatment are available. Your child’s healthcare team will help you as you make important decisions about your child’s health.
What is leukemia?
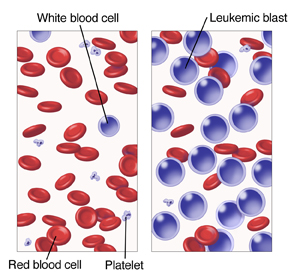
Leukemia is cancer of the bone marrow (the spongy liquid inside of bones) and blood. The blood is made up of 3 main types of cells:
White blood cells that fight infection.
Red blood cells carry oxygen throughout the body to give a person energy.
Platelets that help the blood clot to stop bleeding when a person is injured.
Leukemia usually affects the white blood cells. When a person is healthy, white blood cells form in the bone marrow. With leukemia, large numbers of abnormal white blood cells called leukemic blasts are produced. These blasts live longer than normal white blood cells and crowd out the healthy cells. As time goes on, there are more blasts than healthy cells, so that the blood can’t do its job. This leads to problems, such as infections and bleeding. Anemia can also occur. This is a condition when there are too few red blood cells.
Who gets leukemia?
Leukemia is the most common type of childhood cancer. Children at any age can get leukemia, but younger children are affected most often. Leukemia is not contagious. This means the child can’t pass it to another person.
What causes leukemia?
Leukemia occurs when white blood cells grow abnormally (mutate). What causes this to happen is not fully known. Changes in certain genes, called mutations, may affect the way your child’s cells grow. This gene mutation is random and couldn’t have been prevented. In rare cases, other factors, such as certain inherited conditions or exposure to certain chemicals or radiation, might play a role. But most often, the cause of leukemia in children is unknown.
Types of leukemia
There are many different types and subtypes of leukemia. The main types of leukemia that affect children include the following:
Acute lymphoblastic leukemia (ALL) is the most common form of leukemia in children. ALL occurs when the body makes an abnormal type of white blood cells, called lymphoid blasts. These cells don't grow into healthy white blood cells the way they should. ALL is a fast-growing cancer.
Acute myelogenous leukemia (AML) is the second most common form of leukemia in children. AML occurs when the body makes an abnormal type of white blood cell, called myeloid blasts. These cells don't grow into healthy white blood cells the way they should. Children who have had chemotherapy or radiation treatments in the past have an increased risk of AML.
Chronic myelogenous leukemia (CML) is rare in children. CML occurs because the body makes abnormal myeloid cells. With CML, the white blood cells are more mature, but there are too many of them. CML develops more slowly than AML.
Juvenile myelomonocytic leukemia (JMML) is another rare type of leukemia in children. It begins from myeloid cells, but it usually doesn't grow as fast as AML or as slowly as CML.
Your child's healthcare provider will talk with you about the type your child has.
What are the symptoms of leukemia?
Some common symptoms of leukemia include:
Fever
Infections that don't go away
Pale skin
Bruising or bleeding easily
Bone or joint pain
Swollen lymph nodes
Swelling in the abdomen (belly)
Flat red dots on the skin that look like a rash
Tiredness (fatigue)
Weakness
Weight loss
Not every child has all of these symptoms.
How is leukemia diagnosed?
The healthcare provider will examine your child. You will be asked about your child’s health history. Your child may also have one or more of the following:
Blood tests to take samples of blood and examine them under a microscope
Bone marrow aspiration and biopsy to take a sample of bone marrow from the hipbone
Lumbar puncture, also called spinal tap, to take a sample of the fluid that surrounds the spinal cord from the child’s lower back
How is leukemia treated?
Chemotherapy (“chemo”) is the main treatment used for most types of leukemia. It destroys cancer cells with powerful cancer-fighting medicine. The kind of chemo medicine your child receives depends on the type of leukemia your child has. Your child may receive a combination of chemo medicines. The medicines may be given by mouth, injection, or through a tube (IV) that’s usually put into a vein in the arm or chest. Some children might benefit from high-dose chemotherapy followed by a stem cell transplant. Your child’s healthcare provider can tell you more.
Children with CML typically get a type of drug called a targeted therapy, which attacks specific problems inside the CML cells.
Radiation may be part of the treatment plan. Surgery is rarely used to treat leukemia.
Supportive treatments
Supportive treatments help protect the child from infection, prevent discomfort, and bring the body’s blood counts back to a healthy range. During your child’s treatment, he or she may be given antibiotics. These medicines help prevent and fight infection. Other medicines may also be given. These help ease side effects caused by chemotherapy such as nausea. Your child may also receive a blood transfusion to restore the blood cells. The blood cells can't grow because of the leukemia or the effects of the treatments. For blood transfusion, blood is taken from a donor and stored until the child is ready to get it.
What are the long-term concerns?
Leukemia is usually curable with treatment. But chemotherapy may cause some problems, such as damage to certain organs. Your child’s health will need to be watched closely for life. This may include clinic visits, blood tests, and ultrasounds of the heart. Most children cured from leukemia can expect to live typical lives even though they may require some extra medical attention and may have some long-term medical issues.
Call your child’s healthcare provider
Unless advised otherwise by your child’s healthcare provider, call the provider right away if:
Your child has a fever of 100.4°F (38°C) or higher. Get medical care right away.
Your child is fussy or cries and can't be soothed.
Also call your child's healthcare provider right away if your child has any of these:
Chills
Cough
Pain that can’t be controlled
Uncontrolled nausea or vomiting
Weakness
Diarrhea
Coping
Receiving a cancer diagnosis for your child is scary and confusing. Remember that you are not alone. Your child’s healthcare team will work with you and your child throughout your child’s illness and care. You may also want to seek information and support for yourself. Doing so can help you cope with the changes cancer brings. Learning about your child's cancer and talking with others who also have a child with cancer may help you and your family cope with the changes cancer brings. Some helpful resources include:
Children's Oncology Group
https://childrensoncologygroup.org/index.php/patients-and-familiesThe Children’s Leukemia Research Association
www.childrensleukemia.orgThe Leukemia & Lymphoma Society
www.leukemia-lymphoma.org
Updated:
August 08, 2018
Sources:
Fever in children, Up To Date, Neutropenia and fever in people being treated for cancer, Up To Date
Reviewed By:
Image reviewed by StayWell medical illustration team.,Levy, Adam S., MD,Stump-Sutliff, Kim, RN, MSN, AOCNS