When Your Child Has Heat Rash (Prickly Heat)
When Your Child Has Heat Rash (Prickly Heat)
What causes heat rash?
Heat rash is caused by blocked sweat glands. This can happen when your child:
Is exposed to too much sun or heat
Is overdressed (wearing too many layers of clothing)
Engages in intense exercise or physical activity
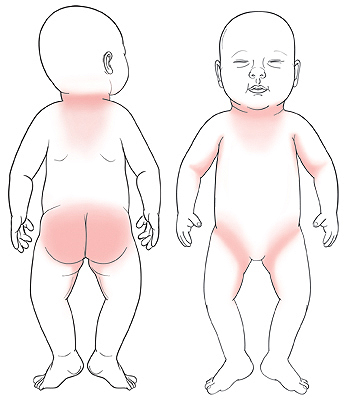
What are the symptoms of heat rash?
Heat rash can cause areas of the skin to turn red, develop small bumps, and become itchy.
How is heat rash diagnosed?
Heat rash is diagnosed by how it looks. To get more information, the healthcare provider will ask about your child’s symptoms and health history. The healthcare provider will also examine your child. You will be told if any tests are needed.
How is heat rash treated?
In most cases, heat rash requires no treatment. It generally goes away on its own within 2 to 3 days. You can do the following at home to help relieve your child’s symptoms:
Apply over-the-counter (OTC) hydrocortisone cream 1 to 2 times per day to the rash to relieve itching. Don't apply the steroid cream under the diaper. Each time before and after applying the cream, wash your hands with warm water and soap.
Give your child OTC antihistamine medicine to relieve itching.
Apply a cool compress (such as a clean washcloth dipped in cool water) to the rash.
Give your child cool baths.
Loosen your child’s diaper if it rubs against the rash area.
Call the healthcare provider
Contact the healthcare provider if your child has any of the following:
A heat rash that doesn’t go away within 7 days of starting treatment
Other symptoms such as a fever, sore throat, or body aches, which may suggest an illness or infection
Fever (see Fever and children, below)
A seizure caused by the fever
Fever and children
Always use a digital thermometer to check your child’s temperature. Never use a mercury thermometer.
For infants and toddlers, be sure to use a rectal thermometer correctly. A rectal thermometer may accidentally poke a hole in (perforate) the rectum. It may also pass on germs from the stool. Always follow the product maker’s directions for proper use. If you don’t feel comfortable taking a rectal temperature, use another method. When you talk to your child’s healthcare provider, tell him or her which method you used to take your child’s temperature.
Here are guidelines for fever temperature. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Infant under 3 months old:
Ask your child’s healthcare provider how you should take the temperature.
Rectal or forehead (temporal artery) temperature of 100.4°F (38°C) or higher, or as directed by the provider
Armpit temperature of 99°F (37.2°C) or higher, or as directed by the provider
Child age 3 to 36 months:
Rectal, forehead, or ear temperature of 102°F (38.9°C) or higher, or as directed by the provider
Armpit (axillary) temperature of 101°F (38.3°C) or higher, or as directed by the provider
Child of any age:
Repeated temperature of 104°F (40°C) or higher, or as directed by the provider
Fever that lasts more than 24 hours in a child under 2 years old. Or a fever that lasts for 3 days in a child 2 years or older.
How is heat rash prevented?
You can help prevent your child from getting a heat rash by:
Removing extra layers of clothing from your child when it’s warm. Children should not wear more than one extra layer of clothing than adults.
Dressing your child in loose-fitting clothing that does not rub against the skin.
Changing your child’s diaper right away when it’s wet or soiled.
Updated:
October 08, 2017
Sources:
Hydrocortisone (Topical): Pediatric Drug Information, UpToDate
Reviewed By:
Adler, Liora C., MD,Dozier, Tennille, RN, BSN, RDMS,Turley, Ray, BSN, MSN