When Your Child Has Coarctation of the Aorta (COA)
When Your Child Has Coarctation of the Aorta (COA)
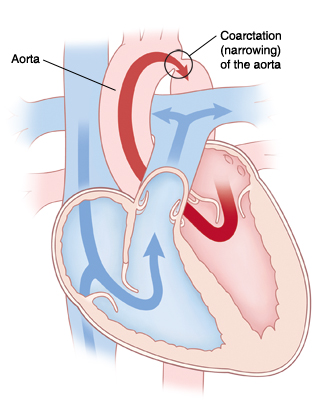
Your child has been diagnosed with coarctation of the aorta (COA). COA is a narrowing in the aorta. The aorta is the main blood vessel that carries blood from the heart to the rest of the body. COA can lead to worsening heart function over time. Current treatments are quite effective for this condition.
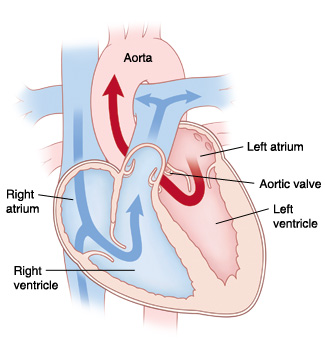
The normal heart
The heart is divided into 4 chambers. The 2 upper chambers are called atria. The 2 lower chambers are called ventricles.
In a normal heart, oxygen-poor blood returning from the body fills the right atrium. This blood flows through the tricuspid valve into the right ventricle. The right ventricle pumps this blood across the pulmonary valve through the pulmonary artery to the lungs to receive oxygen. Oxygen-rich blood from the lungs fills the left atrium. This blood flows through the mitral valve into the left ventricle. The left ventricle pumps this blood across the aortic valve through the aorta to deliver oxygen to the body.
Why is coarctation of the aorta a problem?
With COA, the left ventricle has to work harder than usual to pump blood to the body. This is because there’s reduced blood flow due to the narrowed area in the aorta. Over time, the extra work tires the left ventricle and causes the heart muscle to weaken. It can also cause the muscle to thicken (hypertrophy). In the most extreme cases, your child can develop congestive heart failure (CHF). This is a condition in which the heart can no longer pump blood effectively.
Blood pressure measures the force of moving blood as it pushes against blood vessel walls. High blood pressure (hypertension) occurs when blood pushes with more force than normal. Low blood pressure (hypotension) occurs when blood pushes with less force than normal. COA causes high blood pressure in the upper body and low blood pressure in the lower body. This is because the pressure is higher in the arteries in the area before the narrowing. These arteries send blood to the head and arms. The pressure is lower in the arteries in the area after the narrowing. These arteries send blood to the abdomen and legs. Problems with blood pressure can lead to complications, such as stroke, kidney failure, and intestinal damage.
What causes coarctation of the aorta?
COA is a congenital heart defect. This means it’s a problem with the heart’s structure that your child was born with. COA occurs more often in families with a history of left-sided heart problems. It also occurs more often in children with certain genetic abnormalities.
What are the symptoms of coarctation of the aorta?
Children with mild to moderate COA may appear to be in normal health and have no symptoms at first. Infants with critical COA generally have severe symptoms. Symptoms can include:
Heavy or rapid breathing
Irritability
Infection of the intestines
Poor growth
Tiredness with exercise (in older children)
Cold extremities (in older children)
Pain in the lower part of the leg while walking (in older children)
Circulatory collapse (child becomes gray, cold, and the heart may stop beating)
Trouble feeding (in infants)
How is coarctation of the aorta diagnosed?
Sometimes, COA can be detected with fetal echocardiography (fetal ultrasound) before a child is born. This is a test that uses sound waves to form a picture of the baby’s heart. This test can be done when the mother is at least 16 weeks pregnant.
Frequently, COA isn’t found before birth. In this case, signs of a heart problem may be found during a physical exam after birth. Possible signs include high blood pressure or poor pulses in the legs.
If a heart problem is suspected, your child will be referred to a pediatric cardiologist (doctor who diagnoses and treats heart problems in children). To confirm a diagnosis of COA, several tests may be done. These include:
Chest X-ray. X-rays are used to take a picture of the heart and lungs.
Electrocardiogram (ECG or EKG). The electrical activity of the heart is recorded.
Echocardiogram (echo). Sound waves are used to create a picture of the heart and look for structural defects and other problems.
Cardiac catheterization. A thin, lighted tube is inserted into a vein and guided to the heart to view the heart's structures.
Cardiac MRI or CT. Magnetic waves or X-rays combined with computer processing technology are used to take pictures of the inside of your child’s heart.
How is coarctation of the aorta treated?
COA is treated with open heart surgery or cardiac catheterization. Surgery may be done using a number of techniques. The exact technique will depend on the degree of narrowing and location on the aorta. Cardiac catheterization is generally done on older children. Your child’s cardiologist will evaluate your child’s heart and discuss the best treatment options with you.
What are the long-term concerns?
After repair of COA, most children can be active and participate in sports and physical activities.
Regular follow-up visits with the cardiologist are needed. The frequency of these visits may decrease as your child grows older. COA may recur in the long-term. Further treatment may be needed when your child is older.
Medicine may be prescribed to treat problems such as high blood pressure. This is common in older children even after repair of COA.
Your child may need to take antibiotics before having any surgery or dental work for 6 months after COA repair. This is to prevent infection of the inside lining of the heart or valves. This infection is called infective endocarditis. Antibiotics should be taken as directed by the cardiologist.
Updated:
October 07, 2017
Sources:
Clinical manifestations and diagnosis of coarctation of the aorta, Up To Date, Management of coarctation of the aorta, Up To Date
Reviewed By:
Ayden, Scott, MD,Bass, Pat F. III, MD, MPH,Image reviewed by StayWell medical illustration team.