Blood and Blood Product Transfusions for Cancer
Blood and Blood Product Transfusions for Cancer
A blood transfusion is when whole blood or more often, parts of the blood are given to a person through an IV (intravenous) line placed in a vein. Whole blood or the parts of the blood used for transfusion are called blood products. The blood usually comes from another person. This person is called the donor.
Understanding blood and blood parts
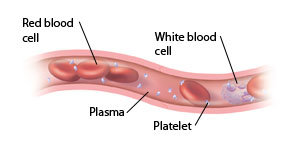
Blood is a fluid that flows throughout the body. It is made up of different parts that have specific roles.
Red blood cells (RBCs) carry oxygen throughout the body.
White blood cells (WBCs) are part of the body’s immune system. Their main job is to help fight infections and diseases.
Platelets are fragments of blood cells that help with clotting. When you have a cut or bruise, platelets come together to form a clot or “plug.” This helps to control bleeding, so you don’t lose too much blood.
Plasma is the liquid portion of blood. It carries the different types of blood cells to all the parts of the body. Plasma also carries proteins called clotting factors. Clotting factors help platelets with the clotting process.
Blood is divided into 4 types: A, B, AB, and O. Blood also has Rh types: positive (+) and negative (–). Any blood products you receive during a transfusion must match with your blood type.
Why a transfusion may be done
Cancer can cause problems that may need treatment with transfusions. For example:
Cancer can affect the bone marrow. This is the soft, spongy part inside the bones where most of the body’s blood cells are made. When the bone marrow is damaged or destroyed, the body can't make enough blood cells. Without enough blood cells, the body can't work normally.
Cancer can cause anemia. This condition happens when there are too few red blood cells in the body. Without enough red blood cells, the body’s tissues and organs don't receive enough oxygen. Anemia can make you feel tired or short of breath.
Occasionally, certain cancers can cause internal bleeding. This can lead to blood loss that can threaten your health.
Certain treatments for cancer can lower the number of healthy blood cells in the body. A transfusion can help increase the number of healthy cells. These treatments include:
Chemotherapy (chemo) uses strong medicines to help kill cancer cells. However, these medicines can also damage healthy cells, including cells in the bone marrow. This can lower your blood cell counts.
Radiation uses strong X-rays to help kill cancer cells. As with chemo, this treatment can also damage healthy cells in the bone marrow. This can lower your blood cell counts.
Surgery may be needed to remove a group of cancerous cells, called a tumor, in the body. The surgery can cause blood loss the need for transfusions.
Types of transfusions
Depending on what you need, your healthcare provider may suggest one or more of the blood products listed below as part of your treatment plan. He or she will explain to you how the transfusions will be given and how often they may be needed. Before receiving any blood products, you will need to have some blood drawn to identify your blood type. You will also need to sign a consent form that says that you understand the potential risks of receiving a transfusion.
RBC transfusions
These are most often used to treat severe anemia or blood loss. RBCs must be “typed” to match your blood type. Except in severe blood loss, people with cancer receive “packed” red blood cells without plasma. Each bag is called a unit. It takes about 2 hours to get 1 unit. During that time, nursing staff will be monitoring your temperature, pulse and blood pressure.
Platelet transfusions
These are used if your platelet count is too low. A low platelet count puts you at high risk of bleeding. Although platelets should be “typed” to match your blood type, it is not needed. Platelets can be obtained in different ways:
From one donor (“apheresis product”)
Combined from several bags of whole blood (“pooled product”)
From a community donor who is specially matched (“matched product”)
It takes about 1 hour or less to get 1 unit of platelets. As with RBCs, nurses will monitor your temperature, pulse, and blood pressure.
Plasma (FFP) transfusions
These may be used to supply the blood with more clotting factors to help stop excess bleeding. FFP must be “typed” to match your blood type. One unit or bag of plasma is taken from a unit of whole blood and is then frozen at the blood bank. Plasma is thawed when it is needed. It usually takes 1 to 2 hours to get 1 unit of FFP.
WBC transfusions
Due to the severe risks involved, these transfusions are rarely used. If there is a problem with the WBCs, your healthcare provider may suggest other treatments to help encourage the growth of new WBCs.
Risks and possible complications of blood and blood product transfusions
These include the following:
Fever and chills
Allergic reaction (itchy skin or rash; redness, or flushing of the face)
Chest pain
Low blood pressure
In the rare event of receiving the wrong blood type:
Back pain
Fast heart rate
Low blood pressure
Nausea
Although extremely rare, some diseases can be transmitted through blood transfusions. They include:
Hepatitis B
Hepatitis C
HIV
Bacterial infections
Learning more about the safety of blood donation and blood transfusions
Strict measures are taken to make sure that donated blood and blood products are safe before they are given to you. To learn more about where donated blood comes from and the process of screening blood, these websites may help:
American Cancer Society, Blood Donation and Transfusion, www.cancer.org/Treatment/TreatmentsandSideEffects/TreatmentTypes/BloodProductDonationandTransfusion/index
American Red Cross, Learn About Blood, www.redcrossblood.org/learn-about-blood
Updated:
June 29, 2018
Sources:
Blood Donation and Transfusion, Up To Date
Reviewed By:
LoCicero, Richard, MD,Sather, Rita, RN