Anemia During Cancer
Anemia During Cancer
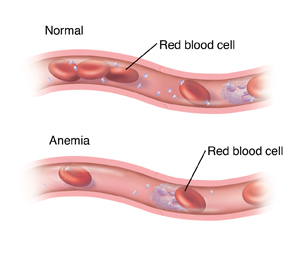
When levels of healthy red blood cells (RBCs) in the body drop to levels that are below normal, the condition is called anemia. Anemia can occur during cancer and its treatment for many reasons. Read below to learn more about anemia during cancer and how it’s treated.
What is anemia?
RBCs are made in the bone marrow. Normally, blood is made up of about 35% to 50% RBCs. Anemic blood has less than 35% RBCs. RBCs carry oxygen around the body. If you have low levels of RBCs, not enough oxygen is delivered to your body. This may cause symptoms of dizziness, weakness, or tiredness. You may have trouble doing daily tasks. You may often feel cold. And you may be short of breath and have a rapid heartbeat. But some people with anemia have no symptoms, especially if the anemia has developed over a long time.
Why anemia can occur with cancer
Anemia during cancer can have several causes. These include:
- Treatments that destroy bone marrow. These include chemotherapy and radiation therapy.
- Some types of cancer that cause blood loss. This includes colon cancer.
- Cancer that destroys the bone marrow. This includes leukemia.
- Blood loss during surgery. Excess blood loss during cancer surgery can cause anemia.
- Low levels of some vitamins and minerals. Not enough B vitamins or iron in your blood can cause anemia.
- Kidney disease. This can lead to low levels of erythropoietin (EPO). This is a substance the body needs to make RBCs.
- Wasting from cancer. Wasting means nutritional problems and weight loss. This lowers the body’s ability to make RBCs.
Testing for anemia
A blood sample is taken from your arm and then tested. Several different types of tests may be done on this blood. Some count the numbers of blood cells. Others test for substances the body uses to make RBCs, such as vitamins and iron.
Treating anemia during cancer
Your treatment will depend on the cause of your anemia. It will also depend on how severe your symptoms are. Your healthcare provider can tell you more about treatment options and their risks and benefits for you. Treatments include the following:
-
RBC transfusion. A tube is put into a vein in the hand or arm. RBCs from a donor are sent through the tube into the body. This increases the number of healthy RBCs in the body. This can reverse anemia very quickly. RBC transfusions are generally safe. But there are some risks. Your healthcare provider will discuss them with you. Be sure you understand these risks. You may need to sign a consent form before receiving treatment.
-
Erythropoiesis stimulating agent (ESA). This is medicine that causes the body to make more RBCs. An ESA is given as a shot. It may be given along with iron (see below). An ESA takes several weeks or months to reverse anemia. There are special risks with ESA treatment. Your healthcare provider will discuss them with you. Be sure you understand these risks. You may need to sign a consent form before receiving treatment.
-
Intravenous (IV) or injection treatments. A liquid medicine with iron is given by shots or IV line. Several treatments may be given. IV iron is often used if you are given an ESA. IV iron usually takes 1 to 4 weeks to reverse anemia. Some vitamins may also be given as an injection (shot), such as vitamin B12.
-
Oral supplements. Iron or vitamin B supplements may be given. These come in liquid or pill form to take by mouth. Or they may be given by injection. Oral supplements can take weeks or months to reverse anemia.
-
Nutritional changes. Eating more foods high in iron and B vitamins may help.
-
Stopping or delaying treatment. Your anemia may improve if you stop or delay chemotherapy or radiation therapy.
Checking your progress
During the course of your treatment, you’ll likely have more blood tests. These are to check your blood levels and your response to the treatment.
Risks and possible complications
Each treatment has its own risks. Your healthcare provider will tell you what risks apply to you. These may include:
-
Fever
-
Hives or other allergic reactions
-
Iron overload
-
High or low blood pressure
-
Nausea
-
Liver inflammation
-
Blood clots
Updated:
March 15, 2019
Reviewed By:
Hanrahan, John, MD,Levy, Adam S, MD