Breast Cancer: Surgery
Breast Cancer: Surgery
Surgery is a common treatment for breast cancer. It’s done to remove as much of the cancer as possible. Women have many surgical options. The type of surgery done depends on:
The size and location of the breast lump or tumor
The type the breast cancer
If the cancer has spread within the breast or has spread outside of the breast to the lymph nodes, or to other parts of the body
The size of the breast
The woman's preference
There are several types of breast surgery. The main types include:
Breast-conserving surgery
Mastectomy
Sentinel lymph node biopsy
Breast reconstruction is surgery to rebuild the breast shape. It can be done after surgery to remove cancer.
Breast-conserving surgery
This type of surgery is also called breast-sparing surgery, lumpectomy, quadrantectomy, partial mastectomy, or segmental mastectomy. The surgeon takes out only the cancer lump and an edge (margin) of healthy tissue around it. The breast itself remains intact.
Radiation therapy is often given after breast-conserving surgery to destroy cancer cells that may not have been removed during surgery. In some cases, chemotherapy and radiation are both given after breast-conserving surgery.
Breast-conserving surgery is a treatment option for some women with small breast cancer that hasn’t spread. Studies have shown that women who have breast-conserving surgery then radiation have similar survival rates as those who have mastectomy. Many women prefer this type of surgery instead of having their whole breast removed.
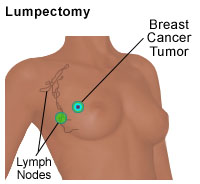
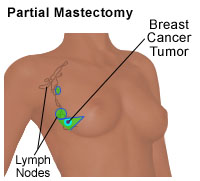
There are 2 main types of breast conservation (tissue-sparing) surgery. These include a lumpectomy and a partial (segmental) mastectomy.
A lumpectomy removes the breast cancer and part of the normal tissue around the cancer. The areas removed during the surgery are shaded in green. The surgeon may also remove some of the lymph nodes under the arm to see if the cancer has spread. The lymph nodes under the arm (called the axillary lymph nodes) drain the lymphatic vessels from the upper arms, most of the breast, the neck, and the underarm areas. Often, breast cancer spreads to these lymph nodes. It can then enter the lymphatic system, and spread to other parts of the body. Radiation therapy is often given after a lumpectomy. This is to kill cancer cells that may not have been removed during the lumpectomy. |
|
A partial (segmental) mastectomy removes the breast cancer and a larger part of the normal breast tissue around the cancer. The areas removed during the surgery are shaded in green. The surgeon may also remove some of the lymph nodes under the arm. The lymph nodes under the arm (called the axillary lymph nodes) drain the lymphatic vessels from the upper arms, most of the breast, the neck, and the underarm areas. Often, breast cancer spreads to these lymph nodes. It can then enter the lymphatic system, and spread to other parts of the body. Radiation therapy is often given after a partial mastectomy. This is to kill cancer cells that may not have been removed during the partial mastectomy. |
Mastectomy
Mastectomy is surgery to remove the breast. The doctor may advise a mastectomy for a woman who has any of the below:
Cancer that has spread to other parts of the breast tissue or has spread to the lymph nodes under the arm
A finished course of radiation therapy to the affected breast or chest area
2 or more areas of cancer in the same breast that are too far apart to be removed with one incision
Breast that is very small and tumor that is large
Inflammatory breast cancer
Connective tissue diseases that are sensitive to radiation therapy
A current pregnancy, because the radiation normally needed after breast-conserving surgery could harm the unborn baby
Some tumor left over from previous breast-conserving surgery
There are 3 types of mastectomy. Your doctor can explain the benefits and risks of each type:
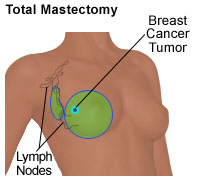
Total (or simple) mastectomy. This type removes the whole breast
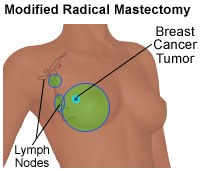
Modified radical mastectomy. This type removes the whole breast, most of the lymph nodes under the arm, and often the lining over the chest muscles. Sometimes the doctor also has to remove part of the chest wall muscles.
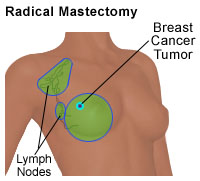
Radical mastectomy. This is also called a Halsted radical mastectomy. This is done in very rare cases. For this surgery, the surgeon removes the whole breast, all of the lymph nodes under the arm, the lining over the chest muscles, and both of the chest muscles under the breast.
A skin-sparing method may be an option for some women planning to have reconstruction surgery at the same time as the mastectomy. This is called immediate breast reconstruction. In this surgery, most of the skin over the breast except the nipple and areola is left intact. The same amount of breast tissue under the skin is removed as with a total mastectomy.
During a total (or simple) mastectomy, the surgeon removes the entire breast. This includes the nipple, the areola, and most of the overlying skin. The areas removed during the surgery are shaded in green. The surgeon may also remove some of the lymph nodes under the arm to see if the cancer has spread. The lymph nodes under the arm (axillary lymph nodes) drain the lymphatic vessels from the upper arms, most of the breast, the chest, the neck, and the underarm areas. Often, breast cancer spreads to these lymph nodes. It then enters the lymphatic system, and spreads to other parts of the body. A skin-sparing mastectomy removes the same amount of breast tissue but leaves most of the skin, except for the nipple and areola. This may be an option if immediate breast reconstruction will be done. |
|
During a modified radical mastectomy, the surgeon removes the entire breast. This includes the nipple, the areola, and the overlying skin. The surgeon also removes some of the lymph nodes under the arm (axillary lymph nodes), and the lining over the chest muscles. In some cases, part of the chest wall muscle is also removed. The areas removed during the surgery are shaded in green. |
|
During a radical mastectomy, the surgeon removes the entire breast. This includes the nipple, the areola, and the overlying skin. The surgeon also removes the lymph nodes under the arm (axillary lymph nodes), and the chest muscles. The areas removed during the surgery are shaded in green. For many years, this was the standard surgery. A radical mastectomy is now rarely done. It is only advised when the breast cancer has spread to the chest muscles. |
Sentinel lymph node biopsy
If breast cancer spreads, it usually spreads first to the lymph nodes under your arm (axillary lymph nodes). Lymph nodes are small bean-shaped organs. They are connected by thin vessels, and drain fluid from the breast area, chest, upper arms, the neck, and underarm area. When breast cancer spreads to lymph nodes, it enters the lymphatic system, and can spread to other parts of the body.
The sentinel lymph node is the node the cancer reaches first. For this surgery, a specially trained surgeon injects a radioactive substance or dye near the tumor. The dye travels to the sentinel node. The node can then be found and removed. It’s then sent to a lab to see if it has cancer cells in it. In some cases, there can be more than 1 sentinel lymph node. If the sentinel node doesn’t have cancer, then it is likely that the rest of your underarm nodes don’t have cancer. Your doctor may opt not to remove other underarm tissue and lymph nodes. Having your underarm lymph nodes removed isn’t a dangerous surgery. But it can lead to side effects, such as numbness due to nerve damage and a lifelong risk of swelling in your arm and chest (lymphedema).
Sentinel lymph node biopsy is a complex surgery. If your doctor thinks you should have this type of biopsy, ask how much experience the surgical team has in the surgery.
This kind of biopsy can save you from having the rest of your nodes taken out. Sentinel node biopsy is often followed by breast-conserving surgery or a mastectomy. This biopsy may be scheduled for the same time as breast-conserving surgery, or it can be done separately.
Risks of breast cancer surgery
All surgery has some risks. The risks of breast cancer surgery include:
Hard tissue in the breast due to scarring at the incision site
Wound infection or bleeding
Breast-conserving surgery may cause:
Short-term (temporary) swelling of the breast
Change in breast size and shape
Clear fluid trapped in the wound (seroma) that may need to be drained and treated with compression or an injection
A risk of lymph node removal is swelling of the arm, hand, chest, and neck (lymphedema). This can cause:
A tight feeling in the arm
Pain
Redness
Decreased flexibility of the arm, hand, and wrist
There may be other risks depending on your overall health and the type of surgery done. Talk with your healthcare provider about any concerns or questions you have about your risks.
Questions to ask your doctor before surgery
Your healthcare team will talk with you the surgery options that are best for you. You may want to bring a family member or close friend with you to appointments. Write down questions you want to ask about your surgery. Make sure to ask:
What type of surgery will be done
What will be done during surgery
The risks and possible side effects of the surgery
If the surgery will leave scars and what they will look like
How your breast or chest will look after surgery
You may also want to ask your doctor other questions, such as:
Which type of surgery do you advise for me? Why?
Where will the cut (incision) be? How much breast tissue will be removed?
Will any lymph nodes be removed?
Will I be able to have breast reconstruction if I have a mastectomy?
Do you advise breast reconstruction to be done at the same time of the mastectomy? Or should it be done at a later date?
Will I need more treatment after surgery, such as radiation or chemotherapy?
What type of follow-up care will I need?
When can I go back to my normal activities?
Getting ready for your surgery
Before surgery, tell your healthcare team if you are taking any medicines. This includes over-the-counter medicines, vitamins, herbs, and other supplements. This is to make sure you’re not taking medicines that could affect the surgery. After you have discussed all the details with the surgeon, you will sign a consent form that says that the healthcare provider can do the surgery.
You’ll also meet the anesthesiologist. This is the doctor in charge of the medicine that helps you sleep and feel no pain during surgery. You can ask questions about the anesthesia and how it will affect you.
After your surgery
You may have to stay in the hospital for a few days, depending on the type of surgery you had. It can also depend on what your insurance will cover. You may want to talk with your insurance company before your surgery.
Your healthcare providers will explain the side effects you can expect with each type of surgery. They can also suggest ways to help prevent or manage these side effects. It is important that you let your healthcare provider know if you have side effects.
After surgery you may have:
Pain. For the first few days after surgery, you are likely to have pain from the incision. Your pain can be controlled with medicine. Talk with your healthcare provider or nurse about your options for pain relief. Some people don’t want to take pain medicine, but doing so can help your healing. If you don’t control pain well, you may not want to cough or move, which you need to do as you recover from surgery.
Tightness in your skin. The skin near your breast may feel tight. Sometimes your arm and shoulder muscles will feel stiff, too.
Fatigue. You may feel tired or weak for a while. The amount of time it takes to recover from surgery is different for each person, but this usually gets better with time.
Recovering at home
When you get home, you may get back to light activity. But you should avoid strenuous activity for 6 weeks. Your healthcare team will tell you what kinds of activities are safe for you while you recover.
After breast cancer surgery, you will have a bandage (dressing) over the place where you had surgery. It is important to keep the surgical area clean and dry. Your doctor will give you specific bathing instructions. If adhesive strips are used, they should be kept dry. They will fall off in a few days.
You may also have tubes in your chest. These are called drains. These are to remove blood and fluids that build up during the healing process. You may have to empty and measure the fluid. Your healthcare team will tell you what problems to look for and tell them about. The drains stay in place for about 2 weeks, or until only a small amount of fluid is draining.
Your doctor or nurse will give you written instructions on how to care for your incision, change your bandage, and drain and check the fluid. You’ll also be told when to call your doctor or nurse about a problem. You should study the instructions and share them with your caregiver, if you have one. Be sure you know how to get in touch with your doctor after hours and on weekends, too.
You may be told to start postmastectomy exercises the day after your surgery, or at a later time. These exercises may include doing things like flexing your fingers and touching your hand to your shoulder. Ask if there are any exercises or activities you should not do to prevent swelling.
Losing one or both of your breasts can be emotionally difficult. After surgery, you and your spouse or partner should take the time to talk about how you feel. You may feel that you need counseling. Ask your healthcare provider for the names and locations of support groups or counselors if you feel you need one.
Possible complications after surgery
After surgery, you may have any of the below. Talk with your healthcare team if you need help.
Stiffness in your underarm after lymph node removal. Gentle exercises and massage therapy can help with stiffness. Don’t use hair removal creams, strong deodorants, or shave under your arm for about 2 weeks after surgery.
Lack of feeling in the skin on your breast or upper arm. When your breast is removed, nerves must be cut. This may cause short-term numbness. Often, most of the feeling returns within 1 to 2 years after surgery. Some numbness may be permanent.
Phantom breast sensations. You may feel like your breast is still there. People who lose limbs often have this feeling, too. The feeling often goes away over time.
Shift in weight or feeling off-balance. If you had large breasts, losing one or both of them can make you feel off-balance and make your neck or back hurt. This often gets better as you adjust to the changes in your body.
Constipation. You may have constipation from using some pain medicine, from not moving much, or from not eating much. Talk with your healthcare provider or nurse about getting more dietary fiber or using a stool softener.
Lymphedema. If you’ve had your underarm lymph nodes removed, you may have swelling in your chest, arm, and hand on the side where you had surgery. While this is normal right after surgery, it can later become a long-term problem. Be sure you understand what to watch for and what to do to help keep this from happening.
Infection. Although not common, infection is a risk whenever you have surgery. Tell your healthcare provider if you have any swelling, redness, warmth, drainage, fever, or sudden pain.
Follow-up care
Your doctor will tell you when to return for a follow-up visit. During this visit, he or she will check the incision and remove stitches if needed.
You may need radiation treatment after surgery. Your healthcare provider will talk with you about this type of treatment.
When to call your healthcare provider
Let your healthcare provider know right away if you have any of these problems after surgery:
Bleeding
Redness, swelling, or fluid leaking from the incision
Fever
Chills
Any other concerns
Updated:
March 13, 2018
Reviewed By:
Levy, Adam S, MD,Stump-Sutliff, Kim, RN, MSN, AOCNS