Asthma Attack
Asthma Attack
Does this describe your symptoms? |
Click image for more info |
Definition
Asthma Triggers: Different things can cause an asthma attack. These are called asthma triggers.
Asthma Medications - There are two main types of asthma medications, long-term and quick-relief:
Peak Flow Meters: Peak flow meters measure how fast an adult can move air out of the lungs. Every adult asthmatic should have a peak flow meter. These measurements are very useful for grading the severity of an asthma attack. The normal peak expiratory flow rate (PEFR) for a healthy adult female is 400-500 and the normal value is 500-650 for a healthy adult male. Peak flow rates decrease during an asthma attack. In general, medications should be increased when the PEFR is less than 80% of baseline and an adult should be seen immediately in the emergency department if the PEFR is less than 50%.
|
When to Call Your Doctor |
Call 911 Now (you may need an ambulance) If |
|
|
|
Call Your Doctor Now (night or day) If |
|
|
|
Call Your Doctor Within 24 Hours (between 9 am and 4 pm) If |
|
|
|
Call Your Doctor During Weekday Office Hours If |
|
|
|
Self Care at Home If |
|
|
HOME CARE ADVICE |
Home Care Advice for Mild Asthma Attack
Quick-Relief Asthma Medicine:
Start your quick-relief medicine (e.g., albuterol or salbutamol) at the first sign of any coughing or shortness of breath (do not wait for wheezing). Use inhaler (2 puffs each time) or nebulizer every 4 hours. Continue the quick-relief medicine until you have not wheezed or coughed for 48 hours.
The best "cough medicine" for an adult with asthma is always the asthma medicine (Note: Don't use cough suppressants, but cough drops may help a tickly cough).
Long-Term-Control Asthma Medicine: If you are using a controller medicine (e.g., inhaled steroids or cromolyn), continue to take it as directed.
Drinking Liquids: Try to drink normal amount of liquids (e.g., water). Being adequately hydrated makes it easier to cough up the sticky lung mucus.
Humidifier: If the air is dry, use a cool mist humidifier to prevent drying of the upper airway.
Hay Fever: If you have nasal symptoms from hay fever, it's OK to take antihistamines (Reasons: poor control of allergic rhinitis makes asthma worse whereas antihistamines don't make asthma worse).
Remove Allergens: Take a shower to remove pollens, animal dander, or other allergens from the body and hair.
Avoid Triggers: Avoid known triggers of asthma attacks (e.g., tobacco smoke, cats, other pets, feather pillows, exercise).
Work with Your Doctor: There is no cure for asthma but you can take charge and learn to control it. The best way to take charge of asthma is to work with your doctor (over many months) to find the right controller (preventive) medicine so your asthma is under control. If you keep having asthma attacks, then the asthma is not under control. People can die from asthma if they do not take it seriously and work with a doctor to control it.
Expected Course: If treatment is started early, most asthma attacks are quickly brought under control. All wheezing should be gone by 5 days.
Call Your Doctor If:
Inhaled asthma medicine (nebulizer or inhaler) is needed more often than every 4 hours
Wheezing has not completely cleared after 5 days
You become worse
How to Use an Inhaler or Spacer
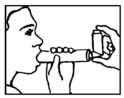
How to Use a Metered Dose Inhaler (MDI):
STEP 1 - Remove the cap and shake the inhaler.
STEP 2 - Hold the inhaler about 1-2 inches (2-5 cm) in front of the mouth. Breathe out - completely.
STEP 3 - Press down on the inhaler to release the medicine as you start to breathe in slowly.
STEP 4 - Breathe in slowly for three to five seconds.
STEP 5 - Hold your breath for ten seconds to allow the medicine to reach deeply into your lungs.
If your doctor has prescribed two puffs, wait 1 minute and then repeat steps 2-5.
How to Use a MDI with a Spacer:
STEP 1 - Shake the inhaler and then attach it to the spacer or holding chamber.
STEP 2 - Breathe out completely.
STEP 3 - Place the mouthpiece of the spacer in your mouth.
STEP 4 - Press down on the inhaler. This will put one puff of the medicine in the holding chamber or spacer.
STEP 5 - Breathe in slowly for 5 seconds.
STEP 6 - Hold your breath for 10 seconds and then exhale.
If your doctor has prescribed two or more puffs, wait 1 minute between each puff and then repeat steps 2-6.
How to Use a Dry Powder Inhaler:
STEP 1 - Remove the cap and follow manufacturer's instructions to load a dose of medicine.
STEP 2 - Breathe out completely.
STEP 3 - Put the mouthpiece of the inhaler in the mouth.
STEP 4 - Breathe in quickly and deeply.
STEP 5 - Hold your breath for ten seconds to allow the medicine to reach deeply into your lungs.
If your doctor has prescribed two or more inhalations, wait 1 minute and then repeat steps 2-5.
Float Test - How to tell if your inhaler (MDI) is EMPTY:
An empty MDI is sometimes the cause of an unresponsive asthma attack.
Most MDIs hold 120 puffs of albuterol or other medicine. It should say on the side of the inhaler.
Shaking the inhaler and hearing fluid in it is not helpful. When the medicine is gone, extra propellant still remains.
The FLOAT TEST: Place the inhaler in a bowl of water and if it floats, assume it's empty. A new and completely full inhaler will sink. The float test is not 100 per cent reliable.
Your Peak Flow Meter
Peak Flow Meter:
Every adult asthmatic should have a peak flow meter.
A peak flow meter is a device that measures how well air moves out of your lungs.
The number that is obtained is called the peak expiratory flow rate (PEFR).
The "personal best" value is the highest PEFR number that a person obtains when they are feeling well.
How to Use a Peak Flow Meter:
STEP 1 - Move the indicator to the bottom of the numbered scale. Stand up.
STEP 2 - Take a deep breath, filling your lungs completely.
STEP 3 - Place the mouthpiece in your mouth and close your lips around it. Do not put your tongue inside the hole.
STEP 4 - Blow out as hard and fast as you can.
STEP 5 - Repeat the process two more times.
STEP 6 - Write down the highest of the three numbers.
Using a Peak Flow Meter to Determine the Severity of an Asthma Attack:
GREEN Zone - MILD Attack: PEFR 80-100% of personal best
YELLOW Zone - MODERATE Attack: PEFR 50-80%
RED Zone - SEVERE Attack: PEFR less than 50%
And remember, contact your doctor if you develop any of the "Call Your Doctor" symptoms.
Updated:
March 22, 2017