DMPS chelation therapy
DMPS chelation therapy
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
2,3-dimercaptopropane-1-sulfonate, British Anti-Lewisite (BAL), calcium disodium ethylenediamine tetra acetic acid (CaNa2EDTA), chelating agents, chelation, chromium, cobalt, Dimaval, dimercaptosuccinate, DMPS, DMSA chelation, D-penicillamine (DPA), EDTA, ethylene diamine tetra-acetic acid,, heavy metal toxicity, lead, lead toxicity, mercury, mercury toxicity, meso 2,3-dimercaptosuccinic acid (DMSA), metal intoxication, metal poisoning, N-acetyl-D-penicillamine (NAPA), unithiol.
Background
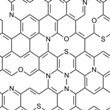
During chelation therapy, chemical compounds and proteins are injected into the blood to treat conditions such as lead toxicity.
Chelation therapy with 2,3-dimercaptopropane-1-sulfonate (DMPS) has been used to treat acute and chronic heavy metal poisoning. It is thought to work by forming an insoluble complex with the metal that is firmly bound to intracellular sites.
Heavy metals such as arsenic, lead, cadmium, and mercury may induce toxic effects in humans due to an imbalance between pro-oxidant and antioxidant homeostasis, termed oxidative stress. Long-term exposure to heavy metals affects normal cellular defense mechanisms and eventually causes apoptosis (cell death). Heavy metals, such as lead and arsenic, interfere with the normal functioning of the central nervous system, hematopoietic system, liver, and kidneys.
Although scientific evidence for effective heavy metal toxicity treatment is not adequate, chelation therapy with chelating agents, such as DMPS and ethylene diamine tetra-acetic acid (EDTA), is considered the best-known treatment for metal poisoning or toxicity.
Both oral and parenteral forms of the substance are available in Europe, but DMPS is only approved in the United States as a bulk chemical. It must be compounded by a pharmacist at the request of the prescribing physician and given as a slow intravenous push. EDTA is another substance used for chelation therapy. EDTA has been approved by the U.S. Food and Drug Administration (FDA) for treating lead poisoning and poisoning from other heavy metals.
Meso 2,3-dimercaptosuccinic acid (DMSA) is another substance used for chelation therapy. According to secondary sources, it has been extensively used in children. Secondary sources suggest that autistic children who received treatment with DMSA for mercury poisoning exhibited marked improvement in their behavioral and cognizant statuses. However, more studies are needed to support these claims.
Agents such as DMPS or DMSA are used in some countries to treat patients with symptoms that are attributed to mercury-containing dental amalgams and in children with autism.
Animal studies suggest that metal toxicity and chelation effects may be influenced by age, which may affect the design of chelation protocols for metal toxicity.
Technique
Chelation agents like 2,3-dimercaptopropane-1-sulfonate (DMPS) and meso 2,3-dimercaptosuccinic acid (DMSA) are available over the counter in some countries. The form of DMPS taken by mouth, Dimaval® (not sold in the United States), is available in 100-milligram capsules.
Some researchers suggest that a combination of antioxidants, herbal extracts, and chelators may be a promising area of future study for heavy metal intoxication.
In general, chelation sessions last about three hours and may be scheduled 1-3 times weekly. Secondary sources suggest that 20-30 sessions may be recommended.
However, there is no standard administration protocol for DMPS. The decision is left up to the discretion of the healthcare provider.
DMPS is thought to work by binding to metal compounds in the body, allowing the body to eliminate them.
Theory/Evidence
Heavy metal toxicity: Chelation therapy with 2,3-dimercaptopropane-1-sulfonate (DMPS) has been used to treat acute and chronic heavy metal poisoning. It is thought to work by forming an insoluble complex with the metal that is firmly bound to intracellular sites.
Arsenic poisoning:Early human evidence suggests that DMPS chelation may help treat arsenic poisoning.
Bismuth poisoning: In a case report, bismuth iodoform paraffin paste (BIPP), used for packing wounds and surgical cavities, resulted in neurological features of bismuth toxicity. After 27 days of intravenous DMPS chelation therapy followed by 24 days of DMPS taken by mouth, symptoms improved and serum and urine concentrations of bismuth decreased.
Cobalt poisoning: Authors of a case report note that chelation therapy with DMPS, ethylene diamine tetra-acetic acid (EDTA), or British Anti-Lewisite (BAL) is a treatment option for chronic cobalt poisoning.
Lead poisoning:DMPS chelation therapy has been used to treat lead poisoning in children. Other chelating agents structurally related to DMPS have been used for lead poisoning in adults following renovation of older homes with lead-based paint and were found to decrease lead levels steadily over several months.
Mercury intoxication: Evidence from small studies and case reports suggest that DMPS chelation therapy may be beneficial for mercury poisoning. However, additional research is warranted.
In a case study, chelation therapy led to considerable clinical improvement of elemental mercury intoxication based on decreased urinary mercury concentration and normalization of electroencephalogram (EEG).
In a controlled study, five patients with long-lasting mercury poisoning showed significant decreases in blood, urine, and cerebrospinal fluid mercury levels after chelation therapy with DMPS.
A study observing the clinical effectiveness of DMPS on the urinary excretion of mercury in 10 occupationally exposed men demonstrated significantly increased mean urine mercury. DMPS was also found to effectively increase urine mercury after treating patients who had chronically applied mercury-containing cream to their skin.
A case report noted the successful use of chelation therapy using DMPS for severe mercury poisoning in combination with continuous venovenous hemodiafiltration (CVVHDF) for kidney support.
A study examining the prognosis of mercury poisoning in mercury refinery workers after removal of exposure and chelation treatment with DMPS demonstrated a reduction in urine mercury and some symptoms, but not in neurological and stomal signs.
In an observational study, DMPS chelation treatment was found to be superior to dimercaptosuccinate (DMS) chelation treatment when there was an elevated urinary mercury level.
In a study observing mercury exposure's effect on a hematological marker, selenoprotein P (Sel-P), DMPS treatment showed no significant decrease.
A case report on thiomersal poisoning determined that DMPS did not substantially influence mercury concentration in blood, urine, or kidney clearance of mercury.
One pharmacology study studied the complexes of mercury and chelating agents (such as DMPS) and concluded that the partition coefficient of the complexes helps explain redistribution of mercury upon administration of antidotes.
In a case study, the use of DMPS plus steroids resulted in full resolution of mercury-induced nephrotic syndrome within six weeks.
Zinc and selenium have been shown to have protective effects against mercury toxicity. However, some evidence suggests that combining zinc or selenium with dithiol chelation agents (such as DMPS) may be counterproductive.
Deliberate metallic mercury injection: Deliberate injection (IV or SC) of metallic mercury is a rare event but has been noted in psychiatric patients, individuals attempting suicide, and as accidental events. In a case report involving a patient who deliberately self-injected with metallic mercury, the course of kidney elimination of mercury, whole blood concentration, and time-course of mercury in the hair was monitored during a five-month treatment period with chelation therapy with DMPS.
In another case report, a patient with intentional IV injection of mercury who was treated with DMPS taken by mouth for five days exhibited slightly enhanced urinary excretion of mercury, but the benefits were considered quantitatively negligible due to deposits that remained in organs.
Autism and autistic spectrum disorders (ASDs): It has been suggested that dietary changes plus DMPS chelation therapy may help improve behavioral, clinical, and biochemical abnormalities in patients with autism. However, conclusive evidence of effectiveness is lacking.
Respiratory disorders: It has been hypothesized that modulation of labile zinc found in conducting airways may influence the production of pro-inflammatory chemokines in respiratory epithelial cells. DMPS was used with good results to modulate the labile zinc, thus regulating gene expression and chemokine production in lung epithelial cells and fibroblasts.
Other unproven uses: A review proposes the added benefits of using supplemental antioxidants in addition to a chelating agent for the treatment of heavy metal toxicity, building on developments in heavy metal poisoning research about the role of oxidative stress and free radicals adding to heavy metal toxicity. This research idea is echoed in another review attempting to determine the role of antioxidant supplementation when using chelating agents such as DMPS and DMSA for arsenic poisoning. Some researchers suggest that the combination of antioxidants, herbal extracts, and chelating agents may be a promising area of future study for heavy metal intoxication. Alpha-lipoic acid and glutathione are examples of antioxidants that are being researched in the treatment of heavy metal toxicities.
Safety
General: Chelation may cause many severe side effects, including allergic reactions, severe kidney damage, bone marrow problems, dangerously low blood pressure, dangerously low calcium levels in the blood, increased risk of bleeding or blood clots, immune reactions, irregular heartbeat, blood sugar imbalances, and convulsions. Death has also been reported, although it is not clear if chelation therapy was the direct cause.
Chelation may be dangerous in people with heart, kidney, or liver disease or with conditions affecting blood cells or the immune system. Use during pregnancy, breast-feeding, or in children may also be dangerous due to potential toxic effects.
In one case report, no side effects were reported during or after 51 days of chelation therapy with 2,3-dimercaptopropane-1-sulfonate (DMPS). A review on the use of antioxidant supplementation during chelation therapy suggests better safety outcomes than the use of chelation therapy alone.
Allergies: A moderate hypersensitivity reaction (rash) to DMPS chelation therapy has been reported.
Stevens-Johnson syndrome (SJS): In a case report, a patient developed a widespread eruption of red, itchy macules over the back and chest after two weeks of therapy with DMPS taken by mouth for chronic mercury vapor exposure. The macules spread and worsened over the next three days. After the patient was diagnosed with SJS, DMPS was stopped, and symptoms gradually improved.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Eyer F, Felgenhauer N, Pfab R, et al. Neither DMPS nor DMSA is effective in quantitative elimination of elemental mercury after intentional IV injection. Clin Toxicol (Phila). 2006;44(4):395-7. View Abstract
Flora SJ, Bhadauria S, Kannan GM, et al. Arsenic induced oxidative stress and the role of antioxidant supplementation during chelation: a review. J Environ Biol. 2007 Apr;28(2 Suppl):333-47. View Abstract
Flora SJ, Mittal M, Mehta A. Heavy metal induced oxidative stress & its possible reversal by chelation therapy. Indian J Med Res. 2008 Oct;128(4):501-23. View Abstract
Guha Mazumder DN. Chronic arsenic toxicity: clinical features, epidemiology, and treatment: experience in West Bengal. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2003 Jan;38(1):141-63. View Abstract
Guha Mazumder DN, De BK, Santra A, et al. Randomized placebo-controlled trial of 2,3-dimercapto-1-propanesulfonate (DMPS) in therapy of chronic arsenicosis due to drinking arsenic-contaminated water. J Toxicol Clin Toxicol. 2001;39(7):665-74. View Abstract
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com
Ovaska H, Wood DM, House I, et al. Severe iatrogenic bismuth poisoning with bismuth iodoform paraffin paste treated with DMPS chelation. Clin Toxicol (Phila). 2008 Nov;46(9):855-7. View Abstract
Richter M, Cantin AM, Beaulieu C, et al. Zinc chelators inhibit eotaxin, RANTES, and MCP-1 production in stimulated human airway epithelium and fibroblasts. Am J Physiol Lung Cell Mol Physiol. 2003 Sep;285(3):L719-29. View Abstract
Rooney JP. The role of thiols, dithiols, nutritional factors and interacting ligands in the toxicology of mercury. Toxicology. 2007 May 20;234(3):145-56. View Abstract
Schneitzer L, Osborn HH, Bierman A, et al. Lead poisoning in adults from renovation of an older home. Ann Emerg Med. 1990 Apr;19(4):415-20. View Abstract
Setz JM, van der Linde AA, Gerrits GP, et al. EEG findings in an eleven-year-old girl with mercury intoxication. Clin EEG Neurosci. 2008 Oct;39(4):210-3. View Abstract
Steens W, Loehr JF, von Foerster G, et al. [Chronic cobalt poisoning in endoprosthetic replacement] [Article in German] Orthopade. 2006 Aug;35(8):860-4. View Abstract
Vallant B, Deutsch J, Muntean M, et al. Intravenous injection of metallic mercury: case report and course of mercury during chelation therapy with DMPS. Clin Toxicol (Phila). 2008 Jul;46(6):566-9. View Abstract
Van der Linde AA, Pillen S, Gerrits GP et al. Stevens-Johnson syndrome in a child with chronic mercury exposure and 2,3-dimercaptopropane-1-sulfonate (DMPS) therapy. Clin Toxicol (Phila). 2008 Jun;46(5):479-81. View Abstract
U.S. Food and Drug Administration (FDA). www.fda.gov
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017