Chelation therapy
Chelation therapy
Natural Standard Bottom Line Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
While some complementary and alternative techniques have been studied scientifically, high-quality data regarding safety, effectiveness, and mechanism of action are limited or controversial for most therapies. Whenever possible, it is recommended that practitioners be licensed by a recognized professional organization that adheres to clearly published standards. In addition, before starting a new technique or engaging a practitioner, it is recommended that patients speak with their primary healthcare provider(s). Potential benefits, risks (including financial costs), and alternatives should be carefully considered. The below monograph is designed to provide historical background and an overview of clinically-oriented research, and neither advocates for or against the use of a particular therapy.
Related Terms
Edetic acid, ethylene diamine tetraacetic acid (EDTA) therapy.
Note: The term "chelation" may be used in general to refer to the use of any chemical in the blood to remove specific contaminants or toxins (for example, deferoxamine is used as a chelating agent to treat high levels of iron in the body). This type of chelation should not be confused with the use of EDTA therapy.
Background
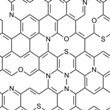
EDTA chelation became well known during the 1950s when it was proposed as a method to cleanse the blood and blood vessel walls of toxins and minerals. The technique involves infusing a chemical called ethylene diamine tetraacetic acid (EDTA) into the blood. The therapy is sometimes given by mouth and occasionally, other chemicals may be used.
Initially, chelation was used to treat heavy metal poisoning. Some observers felt that other benefits occurred in patients receiving this therapy. Currently, chelation practitioners may recommended this treatment for diabetes, for clogged arteries in the heart or legs (called peripheral vascular disease), and for many other conditions. Twenty or more sessions may be recommended and can cost several thousand dollars.
Theory
It has been proposed that treatment with chelation may break down cholesterol plaques in the arteries. Other mechanisms, such as the removal of calcium from these plaques and antioxidant properties, have also been suggested. However, there is little scientific evidence to support these theories.
500-1,000mL of a solution containing 50mg of disodium EDTA per kilogram of body weight is commonly injected into the vein. However, there is no standardized dosage. A single infusion may be used, or multiple infusions may be used daily, over several days or over several weeks.
The American College for the Advancement of Medicine (ACAM) recommends adding heparin, magnesium chloride, a local anesthetic, several B-vitamins, and 4-20g of vitamin C to the chelation solution. This solution is infused slowly over 3.5-4 hours, one to three times a week. The ACAM recommends about 30 treatments for heart disease.
Lifestyle modification, including, stress reduction, caffeine avoidance, alcohol limitation, quitting smoking, exercise and nutritional counseling, is encouraged.
Chelation therapy is rarely administered through the mouth.
Scientific Evidence
Uses These uses have been tested in humans or animals. Safety and effectiveness have not always been proven. Some of these conditions are potentially serious, and should be evaluated by a qualified healthcare provider. |
Grade* |
Heavy metal/lead toxicity For many years, chelation therapy has been used with calcium disodium EDTA to treat heavy metal poisoning. It is still an accepted medical therapy for lead toxicity, and several studies report lower levels of lead in the blood and slower progression of kidney failure. Chelation therapy may also be used to treat iron, arsenic, mercury, or cobalt poisoning. However, some research results are mixed. More studies are needed to clarify. |
B |
Kidney dysfunction Repeated chelation therapy may improve kidney function and slow the progression of kidney damage. Further research is needed to confirm these results. |
B |
Eye disorders (calcific band keratopathy) EDTA is use to treat calcium deposits on the eye. However, well-designed research is needed before a recommendation can be made. |
C |
Ovarian cancer (used with chemotherapy) Early evidence shows that EDTA may be beneficial in ovarian cancer patients when used with chemotherapy. However, further studies are needed before a strong recommendation can be made. |
C |
Heart disease Evidence does not support the use of EDTA chelation therapy in heart disease even though there is strong popular interest in this use. At this time, the evidence suggests it does not work and it cannot be recommended as a treatment for heart disease. |
D |
Claudication (peripheral vascular disease) People with clogged arteries in the legs (peripheral vascular disease) may experience a sensation of pain or fatigue in the legs with exercise (claudication). Studies suggest that EDTA chelation therapy may not be beneficial in claudication and this use is not supported by research at this time. |
F |
*Key to grades:A: Strong scientific evidence for this use; B: Good scientific evidence for this use; C: Unclear scientific evidence for this use; D: Fair scientific evidence against this use (it may not work); F: Strong scientific evidence against this use (it likely does not work). |
|
Tradition/Theory
The below uses are based on tradition or scientific theories. They often have not been thoroughly tested in humans, and safety and effectiveness have not always been proven. Some of these conditions are potentially serious and should be evaluated by a qualified health care professional.
Alzheimer's disease, anemia, arthritis, autism, blood disorders, blood pressure, cataracts, chronic obstructive pulmonary disease (COPD), degenerative diseases (chronic), dementia, diabetes, digoxin toxicity, disease diagnosis, emphysema, encephalopathy, gallstones, gout, heart rhythm abnormalities, hemochromatosis, keratitis (inflammation of the cornea of the eye), macular degeneration, memory loss, neurodegenerative disorders, neuroprotection (oxaliplatin-related toxicity), osteoarthritis, osteoporosis, Parkinson's disease, rheumatoid arthritis, scleroderma, sexual development, sickle-cell disease, snakebites, stroke, systemic lupus erythematosus, vision problems, Wilson's disease.
Safety
Many complementary techniques are practiced by healthcare professionals with formal training, in accordance with the standards of national organizations. However, this is not universally the case, and adverse effects are possible. Due to limited research, in some cases only limited safety information is available.
Chelation therapy may cause serious side effects, such as dangerously low calcium levels in the blood, bone marrow damage that leads to low levels of blood cells, kidney damage (with elevated creatinine levels), very low blood pressure, fast heart rate, increased risk of bleeding or blood clots (including interference with the effects of the blood thinning drug warfarin [Coumadin®]), bacterial blood infections, seizures, allergic or immune system reactions, heart rhythm abnormalities, and unstable blood sugar levels. Other side effects may include fever, nausea, vomiting, gastrointestinal upset, excessive thirst, increased sweating, headache, decreased thyroid function, fatigue, low white blood cell count (leukopenia), low blood platelet count (thrombocytopenia), or inflammation of the uvea (uveitis). Severe reactions have occurred causing people to stop breathing. Although deaths have been reported in people receiving chelation, it is unclear if chelation therapy was the direct cause. One possible cause may be due to the loss of calcium.
Chelation may be dangerous in people with heart, kidney, or liver disease or with conditions affecting blood cells or the immune system. Use during pregnancy, breastfeeding, or in children may also be dangerous due to potential toxic effects.
Author Information
This information is based on a systematic review of scientific literature edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
References
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Anand A, Evans MF. Does chelation therapy work for ischemic heart disease? Can Fam Physician 2003;49:307-309. View Abstract
Anderson TJ, Hubacek J, Wyse, DG, et al. Effect of chelation therapy on endothelial function in patients with coronary artery disease: PATCH substudy. J Am Coll Cardiol 2-5-2003;41(3):420-425. View Abstract
Bell SA. Chelation therapy for patients with ischemic heart disease. JAMA 4-24-2002;287(16):2077-2078. View Abstract
Chappell LT, Stahl JP, Evans R. EDTA chelation therapy for vascular disease: a meta-analysis using unpublished data. J Adv Med 1994;7:131-142.
Ernst E. Chelation therapy for coronary heart disease: an overview of all clinical investigations. Am Heart J 2000;140(1):139-141. View Abstract
Grebe HB, Gregory PJ. Inhibition of warfarin anticoagulation associated with chelation therapy. Pharmacotherapy 2002;22(8):1067-1069. View Abstract
Huynh-Do U. [Gout nephropathy--ghost or reality?]. Ther Umsch 2004;61(9):567-569. View Abstract
Knudtson ML, Wyse DG, Galbraith PD, et al. Chelation therapy for ischemic heart disease: a randomized controlled trial. JAMA 1-23-2002;287(4):481-486. View Abstract
Morgan BW, Kori S, Thomas JD. Adverse effects in 5 patients receiving EDTA at an outpatient chelation clinic. Vet Hum Toxicol 2002;44(5):274-276. View Abstract
Najjar DM, Cohen EJ, Rapuano CJ, et al. EDTA chelation for calcific band keratopathy: results and long-term follow-up. Am J Ophthalmol 2004;137(6):1056-1064. View Abstract
Quan H, Ghali WA, Verhoef MJ, et al. Use of chelation therapy after coronary angiography. Am J Med 12-15-2001;111(9):686-691. View Abstract
Schnabel P, Erdmann E. [Is chelation therapy in coronary heart disease useful?]. Dtsch Med Wochenschr 8-16-2002;127(33):1715. View Abstract
Strassberg D. Chelation therapy for patients with ischemic heart disease. JAMA 4-24-2002;287(16):2077-2078. View Abstract
Villarruz MV, Dans AL, Tan FN. Chelation therapy for atherosclerotic cardiovascular disease [protocol]. Cochrane Database of Systematic Reviews 2002;(4):CD002785. View Abstract
Wong SS, Nahin RL. National Center for Complementary and Alternative Medicine perspectives for complementary and alternative medicine research in cardiovascular diseases. Cardiol Rev 2003;11(2):94-98. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017