What Is Dilated Cardiomyopathy?
What Is Dilated Cardiomyopathy?
Symptoms of dilated cardiomyopathy
Common symptoms include:
Shortness of breath, especially when you exert yourself
Unexplained tiredness
Chest pain
Fluid buildup in the lungs (you may need extra pillows to prop you up so that you can breathe better when you lie down)
Fluid retention causing swollen feet or ankles or unexplained weight gain
Heart skipping beats, fluttering, or thumping
Fainting, dizziness, or lightheadedness
Swelling of the veins of the neck
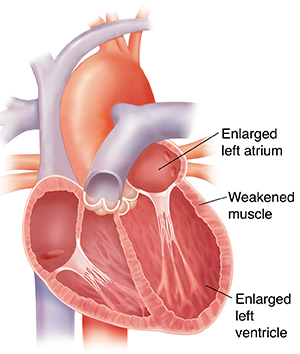
When you have dilated cardiomyopathy
With dilated cardiomyopathy, the heart muscle has been damaged. A damaged heart muscle can't pump as much blood as a normal heart. To try to pump enough blood, the heart muscle stretches so it can hold more. The chambers, especially on the left side of the heart, often dilate (get larger). Larger chambers may help move more blood for a while. But, in time, the stretched-out muscle gets even weaker and tires out. This causes problems with blood delivery to the rest of your body and worsens heart function.
Treatment for dilated cardiomyopathy
Dilated cardiomyopathy doesn’t go away. But it can be treated. Treatment can help keep cardiomyopathy from getting worse, and can reduce your symptoms. Treatment can also help prevent worsening heart failure, blood clots, heart valve problems, and arrhythmias. Your healthcare provider will work with you to develop a treatment plan to help you feel better now and prevent problems in the future. Most often, the symptoms can be managed by medicines and lifestyle changes. Some people have severe symptoms and need to go into the hospital for advanced treatments such as mechanical assist devices or a heart transplant.
Following your treatment plan
Your treatment plan may include:
Making lifestyle changes, such as balancing activity and rest, quitting smoking, and tracking your weight
Eating less salt, as advised
Taking all medicines as prescribed by your healthcare provider
Reducing or eliminating alcohol intake
Keep track of how you feel in a journal
Call your provider right away if you have symptoms that are getting worse.
Be sure to see your healthcare provider regularly. Mention any problems you are having with your treatment plan. Be honest if you are not doing something your provider has suggested. He or she may be able to make some changes to help your plan work better for you.
Updated:
March 21, 2017
Sources:
Yancy, CW., 2013 Guideline for the Management of Heart Failure, Journal of the American College of Cardiology (2013); 62 (16); 93
Reviewed By:
Gandelman, Glenn, MD, MPH,Image reviewed by StayWell medical illustration team.,Snyder, Mandy, APRN