Ventricular Tachycardia (VT)
Ventricular Tachycardia (VT)
What is ventricular tachycardia (VT)?
Ventricular tachycardia (VT) is a fast, abnormal heart rate. It begins in your heart’s lower chambers, called the ventricles. VT is defined as 3 or more heartbeats in a row, at a rate of more than 120 beats a minute. If VT lasts for more than a few seconds at a time, it can become life-threatening. The rapid heartbeat does not give your heart enough time to fill with blood before it contracts again. This can affect blood flow to the rest of your body.
What causes VT?
Ventricular tachycardia occurs when the heart’s electrical system causes the ventricles to beat too fast. Some heart problems can interfere with the heart’s normal electrical system and lead to VT. These include:
- Abnormal heart valves
- Enlarged heart
- Problems with the heart muscles (cardiomyopathy)
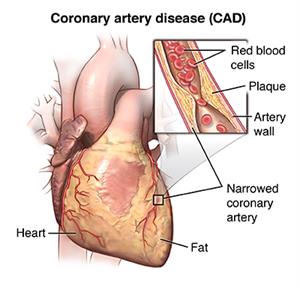
- Clogged arteries (coronary artery disease)
Who is at risk for VT?
VT is often linked to other heart problems that can damage or change normal heart muscle function. Damaged heart muscles can create abnormal electrical circuits that result in VT. You may be more at risk for VT if you have:
- Abnormal heart valves
- Cardiomyopathy
- Congestive heart failure
- Thickened heart muscle, often linked to high blood pressure
- Coronary artery disease
- Had a heart attack
Some types of genetic diseases can also lead to VT. These include:
- Conditions that cause abnormal heart muscle, such as hypertrophic cardiomyopathy
- Diseases that can get inside the heart muscle, such as sarcoidosis
In rare cases, VT occurs when there are no other heart problems.
What are the symptoms of VT?
When you have VT, your heart beats very fast. This may only last for a few seconds. Longer episodes are dangerous. The heart beats so fast that it can’t get enough blood to the rest of your body.
Symptoms of VT may include:
- Fast heartbeat (palpitations)
- Dizziness
- Lightheadedness
- A fluttering feeling in the chest
- Chest pain
- Neck tightness
- Shortness of breath
- Unconsciousness
- Cardiac arrest
In some cases, there are no symptoms at all.
How is VT diagnosed?
To diagnose VT, your healthcare provider may order an EKG (electrocardiogram). This test records your heartbeat’s rate and rhythm. Your provider may want to closely watch your heart’s activity for a longer period of time. Then you may need to use a holter monitor or an event monitor. These are small devices that you wear while doing your normal activities.
In some cases your provider may think you have VT, but hasn’t been able to document it. Then a tiny heart recording device can be implanted into your chest. It can record heart activity for 1 to 2 years.
How is VT treated?
Treatment will depend on your symptoms. No treatment may be needed if:
- You don’t have underlying heart disease
- You are not having difficult symptoms
- Your VT episodes don’t last a long time
If you do have symptoms, your healthcare provider might prescribe medicine (a beta blocker or antiarrhythmic medicine) to control your heart rhythm.
For VT that is long-term (chronic) or life-threatening, an implantable cardiac defibrillator (ICD) may be used. This small device is implanted into your chest. It is connected to your heart with wires. When an abnormal heartbeat occurs, the ICD sends out an electric shock to restore your normal heartbeat.
Some VT may be treated with catheter ablation. This procedure uses radiofrequency energy to destroy the abnormal heart tissue that is causing the rapid heartbeat.
What are the complications of VT?
Some people may have mild symptoms from VT, or no symptoms at all. But for others, VT can be very dangerous. It can lead to sudden cardiac arrest and death.
Can VT be prevented?
VT prevention focuses on treating the underlying heart problems that cause the disorder. This may include:
- Taking medicines for heart failure
- Treating heart artery disease
- Having surgery to fix heart valve problems
- Following a heart-healthy diet and exercise plan, to help reduce your risk for some of these conditions
For some people, caffeine or alcohol can be a trigger for VT episodes. Avoid these things if they affect your VT.
Living with VT
If your healthcare provider diagnoses VT, follow his or her treatment plan closely. Take all medicines as prescribed. And tell your provider about any medicines you may be taking for other health problems. Discuss your alcohol, tobacco, or caffeine use with your medical team. These things can contribute to an irregular heartbeat.
When should I call my healthcare provider?
If you have any of these symptoms, seek immediate medical help:
- Lightheadedness
- Dizziness
- Fainting
- Chest pain
- Persistent rapid heartbeat
Key points about VT
- Ventricular tachycardia (VT) is a fast, abnormal heart rate. This may last for only a few seconds or for a longer period of time.
- VT that lasts for only a few seconds may not need to be treated.
- Longer episodes of VT are dangerous and must be treated.
- Some heart problems can lead to VT.
- Treatment may include medicines or an implantable device to check and correct your heartbeat.
- Seek immediate medical help if you feel lightheaded or dizzy, or have chest pain or a lasting rapid heartbeat.
Next steps
Tips to help you get the most from a visit to your health care provider:
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
April 09, 2017
Sources:
Management of nonsustained ventricular tachycardia. UpToDate., Nonsustained VT in the absence of apparent structural heart disease. UpToDate.
Reviewed By:
Fetterman, Anne, RN, BSN,Kang, Steven, MD