Understanding Bullous Pemphigoid
Understanding Bullous Pemphigoid
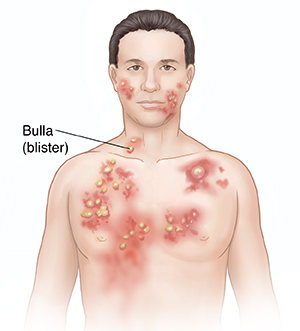
Bullous pemphigoid is a long-term (chronic) skin disease. It mostly affects people ages 60 and older. It causes large blisters to form. These blisters may be on one part of the body or all over. They often appear on the arms, legs, groin, chest, and stomach. Sores may sometimes occur in the mouth, too.
BULL-us PEM-fih-goyd
What causes bullous pemphigoid?
Bullous pemphigoid is an autoimmune disease. That’s when the immune system attacks healthy parts of the body. In this case, it attacks the proteins that join the skin cells to one another. The disease may also be caused by some medicines, such as penicillin.
Symptoms of bullous pemphigoid
Bullous pemphigoid may first look like hives or eczema, because it can be red and itchy. Large, firm blisters may then form. These blisters are often filled with a clear liquid. They may feel very itchy. The blisters may pop. But they usually don’t leave any scars. They may go away and come back again.
Treatment for bullous pemphigoid
The blisters from this skin disease may go away and come back. So treatment is often needed for a few years. Treatment options include:
-
Skin care. Using mild soap and anti-itch creams may help with symptoms.
-
Steroids. Steroids are the main treatment option for this disease. They may be creams or ointments that you put on your skin. Or they may be in pill or liquid form (oral). They can ease itching and stop new blisters from forming. But oral steroids may have side effects.
-
Other medicines. To avoid long term complications of oral steroids, other medications may be added or used instead. Some of these treat the disease by slowing down the immune system.
Possible complications of bullous pemphigoid
-
Skin infection
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as directed
-
Pain that gets worse
-
Symptoms that don’t get better, or get worse
-
New symptoms
Updated:
March 16, 2019
Sources:
Brinster NK, et al. Bullous Pemphigoid. Dermatopathology: High-Yield Pathology. Philadelphia: Saunders; 2011. p. 73-4., Ferri F. Bullous Pemphigoid. In: Ferri F, editor. Ferri's Clinical Advisor 2016. Philadelphia: Elsevier; 2016. p. 263., Leiferman KM. Clinical features and diagnosis of bullous pemphigoid and mucous membrane pemphigoid. Up To Date. October 23 ed: Up To Date; 2014. p. 58., Leiferman KM. Epidemiology and pathogenesis of bullous pemphigoid and mucous membrane pemphigoid. Up To Date. December 28 ed: Up To Date; 2015. p. 20., Murrell D, et al. Management and prognosis of bullous pemphigoid. Up To Date. September 18 ed: Up To Date; 2014. p. 22., Scott M, et al. Bullous pemphigoid. In: Lebwohl MG, editor. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 4 ed. Philadelphia: Elsevier; 2014. p. 108-11.
Reviewed By:
Michael Lehrer MD,Rita Sather RN,Maryann Foley