Parkinson Disease
Parkinson disease (or, simply, Parkinson) is the most common form of Parkinsonism, a group of motor system disorders. It is a slowly progressing, degenerative disease caused by the loss of dopamine-producing brain cells. Dopamine is a substance made in the body that helps with smooth and coordinated muscle movement. Parkinson is usually associated with these symptoms:
- Tremor or trembling of the arms, jaw, legs, and face
- Stiffness or rigidity of the limbs and trunk
- Slowness of movement (bradykinesia)
- Impaired balance and coordination
The cause of Parkinson is unknown. Medical experts believe the symptoms are related to a chemical imbalance in the brain caused by brain-cell death. Parkinson is chronic, and symptoms grow worse over time.
Although the disease may appear in younger people (even teenagers), it usually affects people in late middle age. It is not contagious.
Environmental causes are being researched. Findings have shown that rural living, exposure to well water, and exposure to agricultural pesticides and herbicides are related to Parkinson. It is important to remember, however, that these factors do not guarantee the development of the disease, nor does their absence prevent it. Currently researchers believe that in most people, the cause of Parkinson’s is a mix of genetics and environmental exposure.
In the other forms of Parkinsonism, either the cause is known or suspected, or the disorder occurs as a secondary effect of another neurological disorder. These forms, described as Parkinson syndrome, atypical Parkinson, or, simply, Parkinsonism, may be caused by the following:
- Tumors in the brain
- Repeated head trauma, such as may occur in boxing
- Drug-induced Parkinsonism. This occurs due to the prolonged use of tranquilizing drugs, such as the phenothiazines, butyrophenones, reserpine, and the commonly used drug, metoclopramide for stomach upset.
- Toxin-induced Parkinsonism. This occurs due to manganese and carbon monoxide poisoning.
- Postencephalitic Parkinsonism. A viral disease that causes "sleeping sickness."
- Striatonigral degeneration. The substantia nigra of the brain is only mildly affected, while other areas of the brain show more severe damage.
- Parkinson may accompany other neurological conditions such as Shy-Drager syndrome, progressive supranuclear palsy, Wilson disease, Huntington's disease, Hallervorden-Spatz syndrome, Alzheimer's disease, Creutzfeldt-Jakob disease, olivopontocerebellar atrophy, post-traumatic encephalopathy, and dementia with Lewy bodies.
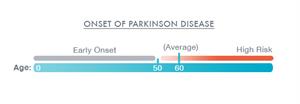
The biggest risk factor for Parkinson is advancing age. The average age for the onset of Parkinson is 60 years. In addition, men are affected more than women. However, the reason for this is unclear.
Family history is another important risk factor. A person with an affected parent or sibling, when compared to the general population, has a 4% to 9% increased chance of developing Parkinson. This increased risk is most likely because of a combination of environmental and genetic factors. Having 1 or more close relatives with Parkinson increases the risk of developing the disease. But, unless there is a known genetic mutation for Parkinson present, the increased risk is 2% to 5%.
These are the most common symptoms of Parkinson:
- Rigid muscles. Stiffness when the arm, leg, or neck is moved back and forth.
- Resting tremor. Tremor (involuntary movement from contracting muscles) that is most obvious at rest.
- Bradykinesia. Slowness in starting movement.
- Postural instability. Poor posture and balance that may cause falls; gait, or balance problems.
Symptoms of Parkinson vary from person to person. The symptoms may appear slowly and in no particular order. Early symptoms may be subtle and may progress over many years before reaching a point where they interfere with normal daily activities.
Other symptoms are divided into motor (movement-related) and non-motor symptoms.
Motor symptoms:- Tremor
- Slow movement (bradykinesia)
- Rigidity and freezing in place
- Stooped posture
- Shuffling gait
- Decreased arm swing when walking
- Trouble getting up from a chair
- Small, cramped handwriting (micrographia)
- Lack of facial expression
- Slowed activities of daily living (for example, eating, dressing, and bathing)
- Trouble turning in bed
- Staying in a certain position for a long period of time
- Diminished sense of smell
- Low voice volume (hypophonia)
- Trouble speaking (dysarthria)
- Painful foot cramps
- Sleep disturbance
- Depression
- Emotional changes (fearful and insecure)
- Skin problems
- Constipation
- Drooling
- Increased sweating
- Urinary frequency or urgency
- Male erectile dysfunction
As the disease progresses, walking may become affected, causing the person to stop in mid-stride or "freeze" in place, and maybe even fall over. People also may start walking with a series of quick, small steps as if hurrying forward to keep balance, a practice known as festination.
The symptoms of Parkinson may look like other conditions or medical problems. Always see your healthcare provider for a diagnosis.
Diagnosing Parkinson in the early stages can be difficult. At first, signs and symptoms may look like other conditions or the effects of normal aging. For this reason, your doctor may want to monitor your symptoms for some time until they are consistently present.
Currently, there are no blood or lab tests to diagnose Parkinson. Diagnosis of Parkinson is based mainly on a medical history and thorough neurological exam. Brain scans or lab tests may be done to help rule out other diseases or conditions, but brain scans generally will turn out to be normal with Parkinson.
Methods to diagnose Parkinson include:
- Neurological exam (including evaluation of symptoms and their severity)
- Trial test of drugs. When symptoms are significant, a trial test of drugs (primarily levodopa [L-dopa]) may be used. If symptoms are relieved from the use of levodopa, this suggests Parkinson.
- Computed tomography scan (also called a CT or CAT scan). An imaging procedure that uses X-rays and a computer to make horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
- Magnetic resonance imaging (MRI). A procedure that uses large magnets, radiofrequencies, and a computer to make detailed images of organs and structures within the body.
So far, there is no cure for Parkinson. However, your doctor can plan appropriate treatment based on the severity of the symptoms and other factors. Treatment may include:
- Medicine
- Surgery
- Complementary and supportive therapies, such as diet, exercise, counseling, stress management, physical therapy, occupational therapy, and speech therapy
Once the diagnosis has been made, the next decision is whether medicine is an option. This depends on:
- The degree of physical and cognitive impairment
- Ability to tolerate antiparkinsonian medicine
- The advice of the doctor and your preferences
No 2 people react the same way to a given drug. It takes time and patience to find the right medicine and dosage to relieve symptoms.
In some cases, your doctor may recommend surgery for Parkinson disease.
Several types of surgery may be done that can help people with Parkinson disease. Most of the treatments are aimed at helping the tremor or rigidity that comes with the disease. In some people, surgery may decrease the amount of medicine needed to control the symptoms of Parkinson.
There are 2 types of surgeries for Parkinson disease:
- Lesion surgery (scarring of tissue). In this procedure, small lesions or scars are made in the deep parts of the brain that help control movement. The surgery may be done while you are awake to help find the exact placement of the lesion. The lesion is placed to help control, or stop, the area of the brain causing the tremor.
- Deep brain stimulation (DBS). With this type of surgery, a small electrode is placed in the deep parts of the brain that help control movement. The electrode is attached to a small battery in the chest wall and is connected by wires that are placed under the skin. The stimulator is then turned on and interrupts the normal flow of information in the brain and can help to decrease symptoms of Parkinson's.
Although Parkinson is a chronic, progressive disease, treatment can help relieve symptoms. It is also important to eat a healthy diet and maintain mobility with the use of assistive devices, if needed. Regular exercise, physical therapy, occupational therapy, and speech therapy can promote independence. Talk with your healthcare provider about depression, anxiety, or other mental health issues that may arise.
- Parkinson is a slowly progressive, degenerative motor system disorder.
- The most common symptoms are muscle rigidity, resting tremor, slowness in initiating movement, and postural instability.
- There is no known cure for Parkinson’s but medications and surgery can help control symptoms.
- Proper diet, regular exercise, physical therapy, occupational therapy, and speech therapy can promote independence.
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
January 16, 2018
Reviewed By:
Hanrahan, John, MD,Dozier, Tennille, RN, BSN, RDMS