Pachyonychia congenita
Pachyonychia congenita
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
Ectodermal dysplasia, Jadassohn-Lewandowsky syndrome, K6a, K6b, K16, K17, keratin, KRT6A, KRT6B, KRT16, KRT17, pachyonychia congenita hereditaria, pachyonychia congenita Jackson-Lawler type, pachyonychia congenital late, pachyonychia congenita recessive, pachyonychia congenita tarda, pachyonychia congenita type I, pachyonychia congenita type II, pachyonychia congenital type III, PC-1, PC-2, PC-3, PC-4.
Background
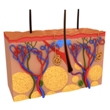
Pachyonychia congenita (PC) is one of the ectodermal dysplasias, a group of syndromes deriving from abnormalities of the ectodermal structures, which include the hair, teeth, nails, sweat glands, cranial-facial structure, and hands. Ectodermal dysplasias are genetic disorders that can be inherited in an autosomal dominant or recessive manner.
While various classifications for PC have been proposed, only two forms of the condition are recognized: type I (PC-1) and type II (PC-2). However, there may be more types of PC, including type III (PC-3), and a form of PC that develops later in life, known as PC tarda, or PC late.
The signs and symptoms of PC typically appear within the first few months of life and include hypertrophic nail dystrophy, which causes the fingernails and toenails to become thickened and abnormally shaped; and palmoplantar keratoderma (painful calluses and blisters on the soles of the feet and, less commonly, on the palms of the hands). Other symptoms include oral leukokeratosis (thick, white patches on the tongue and insides of the cheeks); follicular keratoses, which are bumps that develop around hair follicles on the elbows, knees, and waistline; cysts in the armpits, groin, back, or scalp; and palmoplantar hyperhidrosis (excessive sweating on the palms and soles). Rarely, the condition can affect the larynx (voice box), potentially leading to hoarseness or breathing problems. These complications vary among affected individuals. PC-1 and PC-2 are distinguished by their genetic cause and by their signs and symptoms. Both types are associated with the features described above, but PC-2 has several additional signs that are not typically seen in PC-1. For example, most people with PC-2 develop widespread cysts called steatocystomas during puberty. People with PC-2 are also more likely to have twisted or kinked, brittle, and coarse hair. Additionally, some babies with PC-2 have prenatal or natal teeth, which are present at birth or in early infancy.
Pachyonychia congenita (PC) is a rare genetic disorder that is caused by a single mutation in any one of four keratin genes known as K6a, K6b, K16 or K17. K6a and K6b are located on chromosome 12, while K16 and K17 are located on chromosome 17. Keratin proteins are tough, insoluble, structural proteins that grow from the skin and include hair and nails. Mutations in keratin genes K6a or K16 cause PC-1, while mutations in keratin genes K6b and K17 cause PC-2. PC-1 is more common than PC-2.
PC is an inherited disorder, meaning that is passed down among family members. For both types of the disorder, PC follows an autosomal dominant pattern of inheritance, meaning that only one copy of the defective gene is needed for the disease to appear in either males or females. There have also been reports of PC following a recessive pattern, in which an individual must inherit two copies of the defective gene for the disease to appear.
PC is extremely rare, with only a few reported cases in the United States. The Pachyonychia Congenita Project Mission Statement, which is a consortium of scientists and doctors that works to find a cure for this disease, claims there are fewer than 300 known cases worldwide. There have been clusters of cases in Slovenia, Croatia, China, and Italy. The worldwide incidence is not known but is estimated at 70 cases in 10 million people in Slovenia and 53 cases in 10 million people in Croatia. However, all races and ethnicities are likely to be equally affected. In addition, males and females are affected in equal numbers.
Although there is no cure for PC, it is not a fatal disorder. Treatments aim to reduce symptoms and prevent complications. Individuals with PC have normal life expectancies.
Risk Factors
The only known risk factor for pachyonychia congenita (PC) is a family history of the disease. PC is caused by a mutation or defect in the keratin genes. PC-1 is associated with mutations in keratin genes K6a or K16, while PC-2 is associated with mutations in keratin genes K6b or K17. Information about PC-3 and PC-4 is currently lacking.
It is estimated that in half of all cases, an affected person inherits the mutation from one affected parent in an autosomal dominant pattern. The other cases result from new mutations in the gene and occur in people with no history of the disorder in their family. There have also been reports of PC following a recessive pattern, in which an individual must inherit two copies of the defective gene for the disease to appear.
Causes
General: Pachyonychia congenita (PC) is caused by a mutation or defect in the keratin genes. PC-1 is associated with mutations in keratin genes K6a (KRT6A) or K16 (KRT16), while PC-2 is associated with mutations in keratin genes K6b (KRT6B) or K17 (KRT17). Keratin proteins exist in various forms as the basis for various structures, including hair and nails in humans, but also feathers in birds and hooves in horses. Mutations in any of these genes alter the structure of a keratin protein, which prevents keratins from forming strong, stable networks within cells. Without this network, skin cells become fragile and are easily damaged, making the skin less resistant to friction and minor trauma. Defective keratins also disrupt the growth and function of cells in the hair follicles and nails, which leads to the other features of pachyonychia congenita. Information regarding how the keratin gene is mutated to cause disease is lacking.
Autosomal dominant inheritance: PC is most commonly inherited, or passed down among family members, as a dominant trait. Individuals receive two copies of most genes, one from the mother and one from the father. For a dominant disorder to appear, only one defective copy of the keratin geneis necessary. If one parent has the disorder, there is a 50% chance that his or her child will have the disorder. If both parents have the disorder, there is a 75% chance that their child will have the disorder.
Autosomal recessive inheritance: Rarely, PC occurs as an autosomal recessive trait. In this case, a person must inherit two copies of the defective gene, one from each parent. Individuals who inherit only one copy of the defective keratin genegenerally have no symptoms and are called carriers, because they can pass on the disorder to their children.
If one parent is a carrier, or has only one copy of the defective gene, then each child will have a 50% chance of inheriting one defective gene and also being a carrier. If both parents are carriers, each child has a 25% chance of inheriting two defective genes, a 50% chance of inheriting only one defective gene, and a 25% chance of inheriting neither defective gene. Therefore, if both parents are carriers, about one out of four children will have PC.
Random occurrence: PC may also occur in individuals with no family history of the disorder. This is caused by a mutation or defect in the egg, sperm cells, or developing embryo.
Signs and Symptoms
General: As in most ectodermal dysplasias, the nails, skin, and teeth are affected in patients with pachyonychia congenita (PC). Symptoms associated with the fingernails and toenails persist throughout life, while many of the other symptoms improve with age.
Mouth: People with PC develop leukokeratosis (thick, white patches on the tongue, throat, gums, and insides of the cheeks). This irritation may cause patients with PC to have a hoarse voice. Occasionally, abnormal tooth decay is noted in people with PC. People with PC-2 may also be born with what are known as "natal teeth." These teeth may cause difficulty in breastfeeding and may also become lodged in the airway if one becomes loose and falls out.
Nails: People with PC have hyperkeratotic (thick) nails on the fingers and toes. Nails may be discolored and appear yellow, brown, or gray. The nails frequently separate from the nail beds and fall off, and infections of the nail beds are common. Symptoms associated with the fingernails and toenails are often present at birth or develop during the first year of life.
Skin: The elbows, knees, palms of the hands, and soles of the feet may also be affected in patients with PC. Elbows and knees may develop a rash of raised lesions around the hair follicles. This type of skin lesion may also occur around the temples and eyebrows. The rash is caused by a mutation in the gene that leads to a defect in the production of keratin protein. The palms of the hands and soles of the feet may develop thick scaly patches and blisters. In addition, the palms and soles may sweat profusely.
Patients with PC may develop cysts in the skin. These are more common early in life in patients with PC-2 but may also occur later in life in patients with PC-1. The available literature is unclear on whether there is a difference between PC-1 and PC-2.
Other: Rare symptoms may include cataracts, a cloudiness of the lens of the eye; hair defects such as early hair loss and abnormal hair texture; and early loss of teeth.
Most of the symptoms listed here are specific to PC-1, PC-2, or both, as these are the only recognized subtypes at the present time.
Types of the Disease
General: There are two main types of pachyonychia congenita (PC): PC-1 and PC-2. PC-3 and PC-4 have not been well studied and therefore are mentioned here only briefly. Only PC-1 and PC-2 are recognized as subtypes of this condition.
PC-1: PC-1, also known as Jadassohn-Lewandowski syndrome, is the most common form of the disease and is associated with mutations in keratin genes K6a (KRT6A) or K16 (KRT16). PC-1 is associated with nail symptoms and leukokeratosis (thick, white patches on the tongue, throat, gums, and insides of the cheeks).
PC-2: PC-2, also known as Jackson-Lawler syndrome, is less common than PC-1 and is associated with slightly different symptoms and disease severity. PC-2 is caused by mutations or defects in keratin genes K6b (KRT6B) or K17 (KRT17). PC-2 is associated with natal teeth (teeth that are present at birth) and cystic growths of the skin, but less severe leukokeratosis and other skin symptoms. Patients with PC-2 may also develop cataracts.
PC-3: Some researchers have described a syndrome they call PC-3, which is similar to PC-1 but also includes hair defects and white patches on the corneas of the eyes.
PC-4: A fourth type, PC tarda, develops later in life, sometimes as late as one's 30s. Researchers believe that this type is also inherited as an autosomal dominant trait, meaning that only one copy of the defective gene is necessary for the disease to appear.
Diagnosis
General: For a diagnosis of pachyonychia congenita (PC), doctors typically look for a combination of PC symptoms, which may include hypertrophic nail dystrophy; painful calluses and blisters on the soles of the feet and palms of the hands; leukokeratosis (white patches on the tongue and insides of the cheeks); follicular keratoses, bumps that develop around hair follicles on the elbows, knees, and waistline; cysts in the armpits, groin, back, or scalp; and palmoplantar hyperhidrosis (excessive sweating on the palms and soles).
Biopsy: In a biopsy, a small sample of tissue is taken for analysis in a lab. In a patient with PC, a doctor may take a biopsy of the tissue in the mouth to make sure that the white patches are not cancerous. A biopsy may also be performed on the skin to assess the type and degree of severity of skin conditions.
Genetic testing: If PC is suspected, a genetic test can be conducted to determine whether a person carries a single mutation in any one of four keratin genes known as K6a, K6b, K16, or K17. A sample of the patient's blood is taken and analyzed for the defect in the keratin genes. If this defect is detected, a positive diagnosis is made.
Prenatal DNA testing: If there is a family history of PC, prenatal testing may be performed to determine whether the fetus has the disorder. Amniocentesis and chorionic villus sampling (CVS) can diagnose PC. However, because there are serious risks associated with these tests, patients should discuss the potential health benefits with a medical professional. DNA sequencing can be conducted to determine whether one carries the defective CTSC gene to determine whether there is a risk of the parents conceiving a child with the disease.
During amniocentesis, a long, thin needle is inserted through the abdominal wall and into the uterus, and a small amount of amniotic fluid is removed from the sac surrounding the fetus. Cells in the fluid are then analyzed for normal and abnormal chromosomes. This test is performed after 15 weeks of pregnancy. The risk of miscarriage is about one in 200-400 patients. Some patients may experience minor complications, such as cramping, leaking fluid, or irritation where the needle was inserted.
During chorionic villus sampling (CVS), a small piece of tissue (chorionic villi) is removed from the placenta between the ninth and 14th weeks of pregnancy. CVS may be performed through the cervix or through the abdomen. The cells in the tissue sample are then analyzed for the mutation in the keratin genes. Miscarriage occurs in about 0.5-1% of women who undergo this procedure.
Complications
Voice problems: Rarely, the condition can affect the larynx (voice box), potentially leading to hoarseness or breathing problems. These features vary among affected individuals.
Walking: Individuals with PC can develop very painful calluses and blisters on the soles of the feet and, less commonly, on the palms of the hands. The blistering is most severe in weight-bearing areas and other areas that experience trauma or friction. Severe blistering and callusing on the feet can make it painful or impossible to walk.
Treatment
General: There is no known cure for pachyonychia congenita (PC). Instead, treatment aims to reduce symptoms and prevent complications. In addition, people with PC may be advised not to participate in activities that will aggravate the condition of the nails, such as bowling.
Fluorouracil: This anticancer drug, which blocks the synthesis of an enzyme required for DNA replication, may help decrease the growth of cells that contribute to the nail problems seen in PC.
Retinoids: Retinoids are compounds related to vitamin A, and an example is retinol. Retinoids taken by mouth may help the skin, nail, and mouth symptoms seen in PC, as they have been shown to successfully treat a variety of skin conditions. Minor adverse effects of retinoids include dryness and cracking of the skin, temporary hair loss, and dryness of the eyes, mouth, and nostrils. Severe adverse effects of retinoids may include liver damage, increased blood cholesterol levels, excessive bone growth, and birth defects if taken by pregnant women. Retinoids can also cause birth defects from male transmission of fluids during conception. Retinoids can cause headache and swelling of the brain. People taking retinoids should be regularly monitored for these adverse effects. In addition, women of childbearing age are required to undergo regular pregnancy tests while taking a retinoid.
Skin softeners: Skin softeners or keratolytics, such as salicylic acid, may be used to improve the condition of the skin on the palms of the hands and soles of the feet. Skin softeners may also be used to treat the condition of the nails. Once the nails are softened, they can be cut or filed down more easily.
Surgery: Severely affected nails may be surgically removed. Unless the entire nail bed is removed, the nails will grow back and problems may persist.
Integrative Therapies
Currently there is a lack of scientific evidence on the use of integrative therapies for the treatment or prevention of pachyonychia congenita (PC).
Prevention
General: Because pachyonychia congenita (PC) is an inherited condition, there is currently no known way to prevent the disease. However, a number of options are available for prospective parents with a family history of PC.
Genetic testing and counseling: Individuals who have PC or are carriers of any of the defective keratin genes may meet with a genetic counselor to discuss the risks of having children with the disease. Individuals with family histories of PC may meet with a genetic counselor to determine whether they carry the defective gene. Carriers can be determined through detailed family histories or genetic testing.
Genetic counselors can explain the options and the associated risks of various tests, including preimplantation genetic diagnosis (PGD), amniocentesis, and chorionic villus sampling (CVS).
Preimplantation genetic diagnosis (PGD) may be used with in vitro (artificial) fertilization. In PGD, embryos are tested for the defective keratin genes, and only the embryos that are not affected may be selected for implantation. Because PC can be detected in a fetus, parents may choose whether to continue the pregnancy. Genetic counselors may assist parents with these difficult decisions.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Bowden PE, Haley JL, Kansky A, et al. Mutation of a type II keratin gene (K6a) in pachyonychia congenita. Nat Genet. 1995;10(3):363-5. View Abstract
Chong-Hai T, Rajagopalan DDM. Pachyonychia congenita with recessive inheritance. Arch Dermatol. 1977;113: 685-6. View Abstract
Clementi M, Cardin de Stefani E, Dei Rossi C, et al. Pachyonychia congenita Jackson-Lawler type: a distinct malformation syndrome. Br J Derm. 1986;114:367-70. View Abstract
Haber RM, Rose TH. Autosomal recessive pachyonychia congenita. Arch Dermatol. 1986;122: 919-23. View Abstract
Leachman SA, Kaspar RL, Fleckman P, et al. Clinical and pathological features of pachyonychia congenita. J Invest Dermatol Symp Proc. 2005;Oct;10(1):3-17. View Abstract
Lucker GP, Steijlen PM. Pachyonychia congenita tarda. Clin Exp Dermatol. 1995;20(3):226-9. View Abstract
McLean WH, Rugg EL, Lunny DP, et al. Keratin 16 and keratin 17 mutations cause pachyonychia congenita. Nat Genet. 1995;9(3):273-8. View Abstract
National Foundation for Ectodermal Dysplasias. www.nfed.org.
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Pachyonychia Congenita Project. Mission Statement: Find a cure for Pachyonychia Congenita. www.pachyonychia.org.
Paller AS, Moore JA, Scher R. Pachyonychia congenita tarda. A late-onset form of pachyonychia congenita. Arch Dermatol. 1991;127(5):701-3. View Abstract
Sivasundram A, Rajagopalan K, Sarojini T. Pachyoncychia congenita. Int J Derm. 1985;24: 179-80. View Abstract
Soderqvist NA, Reed WB. Pachyonychia congenita with epidermal cysts and other congenital dyskeratoses. Arch Derm. 1968;97: 31-3. View Abstract
Xiao SX, Feng YG, Ren XR, et al. A novel mutation in the second half of the keratin 17 1A domain in a large pedigree with delayed-onset pachyonychia congenita type 2. J Invest Dermatol. 2004;122(4):892-5. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017