Myeloproliferative disorders
Myeloproliferative disorders
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
Blood disorder, bone marrow, bone marrow transplant, cancer, CML, enlarged spleen, interferons, myelofibrosis, platelets, red blood cells, splenectomy, stem cell transplant, stem cells, thrombocytosis, white blood cells.
Background
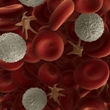
Myeloproliferative disorders are a group of rare illnesses that cause blood cells in the bone marrow, including red blood cells, white blood cells, and platelets, to grow and develop abnormally. Bone marrow is the soft, spongy tissue found inside bones.
There are four major types of myeloproliferative disorders: chronic myelogenous leukemia, essential thrombocytosis, myelofibrosis, and polycythemia vera.
Chronic myelogenous leukemia (CML): Chronic myelogenous leukemia is a cancer of the bone marrow. It occurs when the bone marrow produces abnormal granulocytes (a type of white blood cell). The white blood cells are usually produced normally at first, but they are not able to fully mature and allow new cells to replace them. Normally, white blood cells help fight against diseases and infections. In patients with CML, these white blood cells are unable to function properly. Over time, the white blood cells overcrowd healthy blood cells. Eventually, the bone marrow may become damaged and stop producing white blood cells normally. All of these factors lead to an increased risk of bleeding and developing infections. CML is considered a chronic condition because it usually progresses much slower than acute leukemia.
Essential thrombocytosis: Essential thrombocytosis occurs when the body produces too many platelet cells. These cells help the blood clot in order to stop bleeding. When there is too much clotting in the body, small blood vessels may become clogged. As a result of excessive clotting, blood flow is limited or completely blocked through blood vessels. Depending on where the blockage occurs, the condition may be fatal. For instance, if arteries in the heart are blocked, it may lead to a heart attack.
Myelofibrosis: Myelofibrosis, also called myelosclerosis, occurs when the bone marrow produces too much collagen or fibrous tissue. As a result, fewer blood-producing cells are created, and they can be destroyed more rapidly, which leads to anemia (low levels of red blood cells), low platelet count, and an increased risk of developing infections. This condition can occur by itself or in combination with other myeloproliferative disorders, such as essential thrombocytosis or polycythemia vera.
Polycythemia vera: Polycythemia vera occurs when the bone marrow produces too many blood cells, especially red blood cells. This condition may cause the blood to become thicker than normal, which can impair the functions of vital organs, such as the brain or heart.
The cause of myeloproliferative disorders remains unknown, although some researchers believe that genetics and exposure to certain chemicals, radiation, and electrical wiring may play a role.
Myeloproliferative disorders are serious medical conditions. Complications of these disorders may be fatal. A person's survival rate depends on the type of myeloproliferative disorder he/she has, as well as the severity of his/her illness. For instance, myelofibrosis may lead to death within three to six years. On average, people with CML live about four to five years after diagnosis. However, if CML progresses into acute leukemia, the average survival rate is only three months. People with other, less severe types of myeloproliferative disorders can often live much longer, especially if they are diagnosed in the early stages of the disease. People with polycythemia vera live an average of 10-20 years after diagnosis. People with primary thrombocytosis generally have a normal life expectancy with only a low risk of developing cancer.
Although there is no cure for myeloproliferative disorders, treatment may help patients live several years after they are diagnosed.
Causes
General: Myeloproliferative disorders occur when the body produces too many of one or more types of blood cells. However, the reason for this remains unknown. Researchers believe that genetics and/or the environment may play a role in the development of these disorders.
Genetics: Some people with chronic myelogenous leukemia (CML) have been shown to have a shortened chromosome, called the Philadelphia chromosome. Chromosomes contain a person's genetic makeup, called DNA. This abnormality suggests that genetics may play a role in some types of myeloproliferative disorders.
Signs and Symptoms
General: Many patients with myeloproliferative disorders do not have any symptoms, and they are often diagnosed during a routine examination. Nearly all types of myeloproliferative disorders (except essential thrombocytosis) may cause an enlarged spleen, because the extra blood cells are stored in this organ. An enlarged spleen often causes symptoms of abdominal pain and a feeling of fullness.
Chronic myelogenous leukemia (CML): Early symptoms of chronic myelogenous leukemia (CML) may include fever, weight loss or decreased appetite, fatigue, pain or fullness in the left side of the abdomen, and night sweats.
In the more advanced stages of the disease, patients may have shortness of breath, anemia, enlarged spleen, pale skin, frequent infections, increased risk of bleeding, bruising easily, bone pain, joint pain, or small purple or red dots on the skin (called petechiae).
Essential thrombocytosis: Symptoms of essential thrombocytosis may include headache, burning or throbbing pain in the skin, bruising easily, swelling in the hands and feet, and gastrointestinal bleeding (which may be indicated by blood in the stools)
Myelofibrosis: Symptoms of primary myelofibrosis may include fatigue, general feeling of discomfort, difficulty breathing, weight loss, fever and night sweats, anemia, and abnormal bleeding.
Polycythemia vera: Symptoms of polycythemia vera may include fatigue, general feeling of discomfort, difficulty breathing, stomachache, purple spots or patches on the skin, itching after bathing in warm water, headache, vision problems, nosebleeds, bleeding of the gums, bleeding of the stomach (which may be indicated by blood in the stools), and throbbing and burning pain in the skin.
Diagnosis
General: A myeloproliferative disorder may be suspected if a patient has symptoms of one of these disorders. The most common symptom noticed during a physical examination is an enlarged spleen. A doctor may then perform blood tests and a bone marrow biopsy to confirm a diagnosis.
Blood tests: A complete blood count can determine if a person has high or low levels of certain types of blood cells, including red blood cells, white blood cells, and platelets. They can also detect anemia (low levels of red blood cells) and leukemia (abnormal white blood cells that divide uncontrollably).
Bone marrow biopsy: If a myeloproliferative disorder is suspected and there are abnormalities in a person's blood, a bone marrow biopsy may be performed to confirm a diagnosis. During this procedure, a thin needle with a syringe attachment is used to collect a small sample of liquid bone marrow from the hip bone. A larger needle is then inserted to remove a tiny piece of bone marrow. The individual is usually awake during the procedure, but local anesthetics (such as lidocaine) and sedatives (such as midazolam, or Versed®) may be given to reduce pain. The samples are then analyzed to determine if there are abnormal types or numbers of blood cells.
Complications
Chronic myelogenous leukemia (CML): Some people with CML produce too many platelets. Without treatment, this high platelet count (thrombocytosis) may cause excessive clotting of the blood, which may lead to a heart attack or stroke.
Some people with CML may have a shortage of platelet cells. This may result in easy bleeding and bruising, including frequent or severe nosebleeds, bleeding from the gums, or tiny red marks caused by bleeding into the skin (called petechiae).
Normally, white blood cells help fight against diseases and infections. In people with CML, the white blood cells of someone with CML are unable to function properly. Over time, the white blood cells overcrowd healthy blood cells. Eventually, the bone marrow may become damaged and stop producing white blood cells normally. All of these factors lead to an increased risk of excessive bleeding and developing infections.
CML can cause bone pain or joint pain as the bone marrow expands when excess white blood cells accumulate.
Some of the extra blood cells produced in people with CML are stored in the spleen. As a result, the spleen becomes enlarged, causing a feeling of fullness in the abdomen. If the spleen becomes large enough, there is a risk that it might burst. If the spleen breaks open, urgent medical surgery is needed. Without treatment, a ruptured spleen may cause life-threatening bleeding into the abdominal cavity.
Essential thrombocytosis: Individuals with essential thrombocytosis typically have high levels of platelets in their blood. If the blood clots too much, it may lead to a heart attack or stroke.
Myelofibrosis: Patients with myelofibrosis have an increased risk of bleeding. They are also more susceptible to developing infections than healthy individuals. In addition, patients have an increased risk of developing an enlarged spleen. In extreme cases, the spleen may rupture.
Polycythemia vera: Because individuals with polycythemia vera have thicker blood than normal, they have an increased risk of developing blood clots. A blood clot prevents blood from flowing normally throughout the body. A blood clot can be fatal if it blocks blood flow to a vital organ, such as the brain, heart, or lungs.
Patients have an increased risk of developing an enlarged spleen. In extreme cases, the spleen may rupture.
Treatment
General: There is currently no known cure for myeloproliferative disorders. However, many treatments are available to improve symptoms and prevent complications associated with the disorders. With proper treatment, many people are able to live for several years after they are diagnosed.
Phlebotomy: Patients with polycythemia vera often undergo a procedure called phlebotomy. During the procedure, blood is removed from the patient in order to decrease the person's blood cell count. This procedure may also help reduce the risk blood clots, which helps prevent complications, such as a stroke or heart attack. The amount of blood removed depends on the individual's ratio of blood cells to fluid volume. A doctor typically removes about 500 milliliters of blood once or twice a week until the person's blood ratio is lower than 45%. This treatment needs to be repeated in the future because it does not provide lifelong effects. The frequency of treatment depends on the severity of the patient's condition.
Bone marrow transplant: A bone marrow transplant is the only potential cure for patients with chronic myelogenous leukemia (CML). However, not everyone is a candidate for a bone marrow transplant. The transplant must come from a donor whose body tissues are a close biological match to the recipient.
Serious health risks are also associated with the procedure, as with any major surgery. Individuals who have weakened immune systems are at risk of developing graft-versus-host disease after surgery. This condition occurs when the transplanted bone marrow attacks the recipient's weakened immune system. Other recipients may experience graft-versus host disease (GVHD), also called transplant rejection. This occurs when the body's immune system attacks the donated bone marrow. After a bone marrow transplant, patients typically receive the immunosuppressant drug cyclosporine with or without methotrexate or steroids to prevent GVHD. This is because an estimated 90% of bone marrow transplant recipients develop GVHD.
Interferons: Interferons have been used to treat CML in patients who are unable to undergo a bone marrow transplant. Interferon medication is a man-made version of a protein that is involved in the immune system. The body produces interferons to help fight against disease and infection. These proteins stimulate immune cells to destroy cancerous cells. However, interferons are not safe during pregnancy. They may also cause side effects, such as bone pain, headache, vomiting, and fatigue.
Hydroxyurea: Patients with polycythemia vera and essential thrombocytosis may receive a medication called hydroxyurea, which helps reduce the number of platelets in the blood. Hydroxyurea is an antimetabolite that reduces the production of blood cells in the bone marrow. It may also help reduce the risk of complications, such as an enlarged spleen.
Hydroxyurea may also be used to reduce the number of white blood cells and platelets in the blood and improve anemia in patients with myelofibrosis or CML.
Salicylates: A doctor may recommend medications, called salicylates (such as aspirin), to reduce skin redness and burning, which are often associated with polycythemia vera. These medications also lower high body temperatures that may occur with the condition. Low doses may also improve symptoms of headache and burning skin, which may be caused by essential thrombocytosis.
Antihistamines: Antihistamines, such as diphenhydramine (Benadryl®), may help reduce itching associated with polycythemia vera.
Aminocaproic acid: A medication called aminocaproic acid may be prescribed to reduce bleeding caused by essential thrombocytosis. A doctor may also recommend taking this medication before surgery to prevent bleeding.
Chemotherapy: Chemotherapy drugs, such as cytarabine and daunorubicin, may be prescribed to CML patients. These mediations stop the growth of cancer cells, either by killing the cells or preventing them from multiplying. In CML patients, these drugs are taken orally or injected into a vein or muscle. This allows the drugs to enter the bloodstream and reach cancer cells throughout the body.
Common side effects include nausea, vomiting, fatigue, hair loss, anemia, confusion, depression, problems with blood clotting, stomatitis (sores in the mouth), sores in the throat, dry mouth, diarrhea, constipation, loss of appetite, peripheral neuropathy (burning, weakness, tingling or numbness in the hands and/or feet), acne, dry skin, rash, yellow and brittle nails, flu-like symptoms, fluid retention, decreased sperm motility, and reduced sexual hormone production in women. Some chemotherapy drugs may also damage the kidneys and/or bladder. Chemotherapy also destroys healthy immune cells. Therefore, patients undergoing chemotherapy are immunocompromised and susceptible to infections.
Splenectomy: Patients with CML, myelofibrosis, and polycythemia vera may develop an enlarged spleen. If the spleen ruptures (breaks open) or there is a high risk of it rupturing, a doctor may surgically remove the organ.
Stem cell transplant: In extreme cases of myelofibrosis, surgeons may replace a patient's abnormal stem cells (or cells that produce blood cells) in the bone marrow with healthy stem cells from a carefully selected volunteer donor. The donor must have the same blood and tissue type as the recipient. After the procedure, the healthy bone marrow cells circulate and begin to grow and produce healthy blood cells. However, this type of procedure, called a stem cell transplant, is associated with serious health risks, including graft-versus-host disease (transplant rejection) and infection.
Integrative Therapies
Note: Currently, there is a lack of scientific data on the use of integrative therapies for the treatment or prevention of myeloproliferative disorders. The integrative therapies listed below should be used only under the supervision of a qualified healthcare provider, and should not be used in replacement of other proven therapies or preventive measures.
Strong scientific evidence:
Policosanol: Policosanol is a natural mixture that lowers cholesterol. Various studies have investigated the effect of policosanol on platelet aggregation. In general, studies suggest that policosanol aids in platelet aggregation inhibition, which means it helps to prevent blood from clotting.
Avoid if allergic or hypersensitive to policosanol. Use cautiously if taking aspirin or blood pressure medications. Use cautiously with high blood pressure. Use cautiously if pregnant or breastfeeding.
Vitamin K: Vitamin K is found in spinach, broccoli, asparagus, watercress, cabbage, cauliflower, green peas, beans, olives, canola, soybeans, meat, cereals, and dairy products. Warfarin is a blood-thinning drug that inhibits vitamin K-dependent clotting factors. Warfarin is prescribed by doctors for people with various conditions such as atrial fibrillation, artificial heart valves, history of serious blood clots, clotting disorders (hypercoagulability), or placement of indwelling catheters/ports. Usually, blood tests are done regularly to evaluate the extent of blood thinning, using a test for prothrombin time (PT) or International Normalized ratio (INR). The range for the PT/INR depends on the condition being treated. The PT/INR can become elevated for many reasons and sometimes can get dangerously high and increase the risk of serious bleeding. Patients taking warfarin should be aware of these potential causes, which include many drugs that interact with warfarin, liver disorders, or accidental warfarin overdose. Because the effects of warfarin on anticoagulation are usually delayed by several days, the PT/INR may not increase immediately at the time of overdose. If a person's blood becomes too "thin," management should be under strict medical supervision and may include oral or injected vitamin K for warfarin reversal.
Avoid if allergic or hypersensitive to vitamin K. Injection into the muscle or vein should only be done by a healthcare professional; many serious side effects have occurred after injection. Menadiol (type of vitamin K that is not available in the United States) should be avoided with glucose-6-phosphate dehydrogenase deficiency. Conditions that interfere with absorption of ingested vitamin K may lead to deficiency, including short gut, cystic fibrosis, malabsorption (various causes), pancreas or gall bladder disease, persistent diarrhea, sprue, or ulcerative colitis. Avoid if pregnant. Use cautiously if breastfeeding.
Unclear or conflicting scientific evidence:
Aortic acid: Aortic extract is usually manufactured from the hearts of animals, such as sheep, cows, or pigs. Aortic acid is a broad term encompassing several components, including mesoglycan. Currently, there is not enough evidence to determine if aortic acid is an effective therapy for blood clots in the legs (deep vein thrombosis).
Reports of allergic reactions are currently lacking. Due to the heparan sulfate content of mesoglycan, patients with allergies to heparin or heparinoid derivatives should use caution. Use cautiously with bleeding disorders or if taking anticoagulations. Use cautiously with high blood pressure or if taking blood pressure-lowering agents. Avoid if pregnant or breastfeeding.
Garlic: The garlic bulb is made of many cloves that are wrapped in a paper-thin, white skin. It is used both medicinally and as a spice in food. The anti-platelet effects of garlic have been tested in several human trials. Because garlic has been associated with several cases of bleeding, therapy should be applied cautiously (particularly in patients using other agents that may precipitate bleeding).
Avoid if allergic or hypersensitive to garlic or other members of the Lilaceae(lily) family (like hyacinth, tulip, onion, leek, chive). Avoid with a history of bleeding problems, asthma, diabetes, low blood pressure, or thyroid disorders. Stop using supplemental garlic two weeks before and immediately after dental/surgical/diagnostic procedures with bleeding risks. Avoid supplemental doses if pregnant or breastfeeding.
Ginger: The underground above-ground stems of ginger have been used in Chinese, Japanese, and Indian medicine for hundreds of years. Limited available study suggested that ginger may act as an anti-platelet agent in patients with high blood pressure when used in combination with nifedipine. More study is warranted in this area.
Avoid if allergic to ginger or other members of the Zingiberaceaefamily (like red ginger, Alpinia purpurata, shell ginger, Alpinia zeru, green cardamom, and balsam of Peru). Avoid with anticoagulation therapy. Avoid large quantities of fresh cut ginger with inflammatory bowel disease or with a history of intestinal obstruction. Use cautiously before surgery or with gastric or duodenal ulcers, gallstones, heart disease, or diabetes. Use cautiously long-term. Use cautiously in underweight patients. Use cautiously if taking heart medications or sedatives and if driving or operating heavy machinery. Use cautiously if pregnant or breastfeeding.
Grape seed: Grape leaves, sap, and fruit have been used medicinally since the Greek empire. Early human and animal studies show that extracts of grape seed can aid in platelet aggregation inhibition, which means it helps to prevent blood from clotting.
Avoid if allergic or hypersensitive to grapes or other grape compounds. Avoid with bleeding disorders or with active bleeding. Use cautiously if taking drugs that may increase the risk of bleeding. Use cautiously with drugs processed using the liver's "cytochrome P450" enzyme system. Use cautiously with blood pressure disorders or if taking ACE inhibitors. Avoid if pregnant or breastfeeding.
Pycnogenol®: Pycnogenol® is the patented trade name for a water extract of the bark from the French maritime pine, which is grown in coastal southwestern France. Limited human study reports platelet aggregation inhibition in smokers. Pycnogenol® may also aid in prevention of blood clots during long airplane flights in moderate-to-high risk subjects. Edema (swelling) may also be reduced. Further research is needed to confirm these results.
Avoid if allergic/hypersensitive to pycnogenol, its components, or members of the Pinaceae family. Use cautiously with diabetes, low blood sugar levels, or bleeding disorders. Use cautiously if taking lipid-lowering agents, medications that may increase the risk of bleeding, blood pressure-lowering agents, or immune-stimulating or inhibiting agents. Avoid if pregnant or breastfeeding.
Rutin: Rutin is a yellow crystalline flavonol that is found in various plants, especially the buckwheat plant, black tea, apple peels, onions, and citrus. Human study suggests that Venoruton®, in combination with elastic compression or thrombectomy, may help treat thrombosis. Additional study is needed in this area.
Avoid if allergic/hypersensitive to O-(beta-hydroxyethyl)-rutosides or plants that rutin is commonly found in (such as rue, tobacco, or buckwheat). Use cautiously in elderly patients. Use cautiously with skin conditions. Use cautiously if taking diuretics, anticoagulants or medications used to treat edema. Use cautiously if pregnant or breastfeeding.
Seaweed, kelp, bladderwrack: Bladderwrack (Fucus vesiculosus) is a brown seaweed found along the northern coasts of the Atlantic and Pacific oceans and North and Baltic seas. Another seaweed that grows alongside bladderwrack is Ascophyllum nodosum, andit is often combined with bladderwrack in kelp preparations. Laboratory study has found anticoagulant properties in fucans or fucoidans, which are components of brown algae such as bladderwrack. However, high-quality human studies are currently lacking.
Avoid if allergic or hypersensitive to Fucus vesiculosus or iodine. Avoid with a history of thyroid disease, bleeding, acne, kidney disease, blood clots, nerve disorders, high blood pressure, stroke, or diabetes. Avoid if pregnant or breastfeeding.
Shea butter: Shea butter is derived from the nut of the shea tree (Vitellaria paradoxa). In human trials, shea butter was shown to have anticoagulant properties. Additional studies are needed to confirm these findings.
Avoid with known allergy/hypersensitivity to shea butter or its constituents. Use cautiously if allergic to latex. Use cautiously if taking anticoagulants. There is currently insufficient available safety evidence during pregnancy or breastfeeding.
Turmeric: Turmeric (Curcuma longa) is a perennial plant native to India and Indonesia, and it is often used as a spice in cooking. The rhizome (root) of turmeric has long been used in traditional Asian medicine to treat gastrointestinal upset, arthritis pain, and fatigue. Early research suggests that turmeric may aid in blood clot prevention. However, more research is needed to confirm these results.
Avoid if allergic or hypersensitive to turmeric, curcumin, yellow food colorings, or plants belonging to the Zingiberaceae (ginger) family. Use cautiously with a history of bleeding disorders, immune system deficiencies, liver disease, diabetes, low blood sugar levels, or gallstones. Use cautiously with blood-thinners, such as warfarin (like Coumadin®), or blood sugar-altering medications. Avoid in medicinal amounts if pregnant or breastfeeding. Turmeric should be stopped before scheduled surgery.
Vitamin E: Vitamin E exists in eight different forms ("isomers"): alpha, beta, gamma and delta tocopherol; and alpha, beta, gamma and delta tocotrienol. Alpha-tocopherol is the most active form in humans. Data suggests that supplementation with vitamin E may reduce the risk of venous thromboembolism (VTE) in women and in patients with a prior history or genetic predisposition for this condition.
Avoid if allergic or hypersensitive to vitamin E. Avoid with retinitis pigmentosa (loss of peripheral vision). Use cautiously with bleeding disorders or if taking blood thinners. Avoid doses greater than the recommended daily level in pregnant women and breastfeeding women.
Yohimbe bark extract: The terms yohimbine, yohimbine hydrochloride, and yohimbe bark extract are all related. However, they each have a slightly different meaning. Yohimbine is found in the bark of the Pausinystalia yohimbe tree. Yohimbine hydrochloride is a standardized form of yohimbine that is available as a prescription drug in the United States. Yohimbine hydrochloride has been used to treat many medical conditions, such as erectile dysfunction and dry mouth. Preclinical studies report that yohimbine alkaloid, isolated from yohimbe bark, may aid in inhibition of platelet aggregation. Research in humans is limited, and more research is necessary in this area.
Yohimbine is generally well tolerated in recommended doses. However, many side effects have been reported with yohimbine hydrochloride and may apply to yohimbe bark. Avoid if allergic to yohimbe, any of its components, or yohimbine-containing products. Use cautiously with peptic ulcer disease, kidney disease, high blood pressure, heart disease, or if taking drugs that affect blood sugar levels. Avoid with benign prostate hypertrophy (enlarged prostate), anxiety, mania, depression, stress disorders, post-traumatic stress disorders, bipolar disorders, or schizophrenia. Avoid use in children or in pregnant or breastfeeding women.
Fair negative scientific evidence:
Boron: It has been proposed that boron may affect the activity of certain blood clotting factors. However, study results conflict regarding boron's specific coagulation effects. Additional research is needed to form a clear conclusion.
Avoid if allergic or sensitive to boron, boric acid, borax, citrate, aspartate, or glycinate. Avoid with a history of diabetes, seizure disorder, kidney disease, liver disease, depression, anxiety, high blood pressure, skin rash, anemia, asthma, or chronic obstructive pulmonary disease (COPD). Avoid with hormone-sensitive conditions like breast cancer or prostate cancer. Avoid if pregnant or breastfeeding.
Prevention
The cause of myeloproliferative disorders is poorly understood. Therefore, there is no guaranteed way to prevent these conditions. However, avoiding or minimizing exposure to certain chemicals (such as hair dyes), radiation, and electrical wiring may help reduce the risk of developing myeloproliferative disorders.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Becze E. The future is now for the treatment of chronic myelogenous leukemia. ONS Connect. 2007;22(8 Suppl):69-70. View Abstract
Enright H, McGlave PB. Chronic myelogenous leukemia. Curr Opin Hematol. 1996 Jul;3(4):303-9. View Abstract
Guilhot F. The role of interferon in the treatment of chronic myelogenous leukemia in chronic phase. Nouv Rev Fr Hematol. 1994;36 Suppl 1:S39-46. View Abstract
Kantarjian HM, O'Brien S, Smith TL, et al. Treatment of Philadelphia chromosome-positive early chronic phase chronic myelogenous leukemia with daily doses of interferon alpha and low-dose cytarabine. J Clin Oncol. 1999 Jan;17(1):284-92. View Abstract
Kowata S, Ishida Y. [Diagnostic approach to thrombocytosis.] [Article in Japanese.] Nippon Naika Gakkai Zasshi. 2007 Jul 10;96(7):1363-7. View Abstract
National Cancer Institute (NCI). www.cancer.gov.
National Institutes of Health (NIH). www.nih.gov.
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
No authors listed. [Pathophysiology of and therapy for primary myelofibrosis.] [Article in Japanese.] Nippon Naika Gakkai Zasshi. 2007 Aug 10;96(8):1724-32. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017