Long QT Syndrome
Long QT Syndrome
What is long QT syndrome?
Long QT syndrome (LQTS) is a disease that you can inherit or acquire. It affects the bottom pumping chambers of the heart (ventricles). It can cause a dangerous rapid heart rate and abnormal rhythm.
The heart has both muscular and electrical components. When electricity flows through the heart muscle, it is triggered to squeeze or beat. Heart muscle cells use highly coordinated ion channels to regulate the flow of electricity to generate normal heartbeats. Ion channels are what the electrolytes potassium, sodium, and calcium flow through within the heart's cells. In LQTS, a problem in the ion channels leads to electrical instability. This can cause a very rapid and dangerous heart rhythm that can lead to fainting or sudden death. The arrhythmias are called ventricular tachycardia or ventricular fibrillation.
The name long QT stems from a reading on the electrocardiogram (ECG) machine. Healthcare providers use this to evaluate your heartbeat. The ECG machine records and measures each of your heartbeats as 5 “waves.” Each wave has a different letter designation: P, Q, R, S, and T. The relationship between the Q and T waves is important and is known as the QT interval. When the interval lasts longer than it normally should, it disrupts the timing of your heartbeat and can cause dangerous arrhythmias, or irregular heart rates.
What causes long QT syndrome?
Often, LQTS is genetic — passed down through families. Only one parent needs the genetic defect for it to be passed on to the child. If one of your family members is diagnosed with LQTS, experts recommend that you and your other family members — parents, siblings, children — get tested as well.
In rare instances, certain medicines can cause acquired LQTS. The medicines may affect the ion channels in the heart or cause electrolyte problems such as low potassium and calcium. More than 50 drugs list LQTS as a risk. Ask your healthcare provider about the risks of all medicines you're taking.
Who is at risk for long QT syndrome?
If you have a family history of LQTS, you are at risk of developing it.
Specialists believe that if you are susceptible to long QT syndrome, you are more likely to be affected by medicines that increase your risk for the condition. Medicines, such as antibiotics, antidepressants, antihistamines, diuretics, heart medications, and others may increase your risk for LQTS.
What are the symptoms of long QT syndrome?
Some people with LQTS have no symptoms. The condition is detected on an electrocardiogram or heart monitor done for other reasons.
If ventricular arrhythmias do occur, some symptoms include:
- Palpitations or chest fluttering
- Shortness of breath
- Lightheadedness that comes and goes
- Near fainting or fainting
- Cardiac arrest
How is long QT syndrome diagnosed?
An electrocardiogram (ECG) is the main way to detect LQTS. If your healthcare provider notes that the interval between the Q and T waves of your heartbeat is longer than it should be, you may have LQTS. Sometimes the QT interval can change with activity. You may be given a holter monitor, a portable, wearable ECG recording device. You can wear the holter monitor over several days to get readings during different activities. Another option is having an ECG during exercise (exercise stress testing). QT shortening is a normal response to exercise.
Genetic testing is available for inherited LQTS. It may help identify genetic defects associated with LQTS. It may also be used to screen first-degree relatives for the condition.
How is long QT syndrome treated?
For acquired LQTS, correcting any electrolyte problems or changing medicines may be all that is needed.
There is no cure for inherited LQTS, but treatment helps prevent symptoms and minimizes risk for fainting or cardiac arrest. Your doctor may prescribe medicines called beta blockers to reduce arrhythmias.
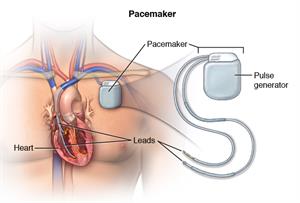
If you continue to have recurrent arrhythmias, or have had cardiac arrest, you may need an implantable cardiac defibrillator (ICD). This device is implanted underneath the skin in the front of the chest wall. A wire connects the device to the heart. The ICD monitors your heart rhythm and if needed, can deliver 1 or more brief electrical shocks to the heart to reset the rhythm.
Surgery is another option for some people with inherited LQTS. It involves removing certain nerves in your chest that influence the heart rhythm.
How is long QT syndrome prevented?
You can't prevent inherited LQTS but you can reduce risk factors that can trigger arrhythmias and sudden death.- See your doctor regularly.
- Take your medicines as prescribed.
- Follow restrictions on certain activities such as strenuous exercise and driving.
- Avoid high-stress situations that may trigger LQTS.
- Ask your doctor if you need a potassium supplement.
- Wear a medical alert bracelet.
When should I call my healthcare provider?
Seek medical attention right away if you:- Have recurrent fainting or near fainting despite treatment with medication
- Receive a shock by your ICD
Key points
- Long QT syndrome is a rare heart disorder that disrupts the electrical activity of your heart.
- This electrical disruption can cause an abnormal heartbeat and even sudden death.
- Family history of long QT syndrome is the main risk factor for developing the condition.
- Medicine or an implantable cardioverter defibrillator (ICD) can help manage the condition.
- Long QT syndrome is potentially fatal and requires medical help.
Next steps
Tips to help you get the most from a visit to your health care provider:
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
April 08, 2017
Sources:
Genetics of Congenital and Acquired Long QT Syndrome, Up To Date
Reviewed By:
Fetterman, Anne, RN, BSN,Kang, Steven MD