Incontinentia pigmenti
Incontinentia pigmenti
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
Bloch-Siemens incontinentia pigmenti melanoblastosis cutis linearis, Bloch-Siemens-Sulzberger syndrome, Bloch-Sulzberger disease, Bloch-Sulzberger syndrome, incontinentia pigmenti type 2, IP, NEMO, neurocutaneous condition, pigmented dermatosis Siemens-Bloch type, skin pigmentation disorder, X-linked inherited disorder.
Background
Incontinentia pigmenti (IP) is one of several ectodermal dysplasias, which are disorders that affect the outer layer of a developing embryo. This layer, called the ectoderm, develops into many parts of a baby's body, including the eyes, skin, nails, and hair. In ectodermal dysplasias, these parts may not develop normally.
IP is a rare inherited genetic disorder that is similar to a condition called hypomelanosis of Ito (HI), formerly known as IP type 1 or IP1. The characteristic feature of HI is hypopigmentation, or the lack of melanin, the pigment that gives color to the skin and hair, resulting in only a little or no color in the skin and hair. Unlike HI, IP presents with skin discoloration caused by excessive deposits of melanin. In IP, melanin collects in the skin, causing wavy lines and streaks that are gray, blue, or brown in color. Many people classify HI as a "negative image" of IP. IP is often referred to as a neurocutaneous condition because it affects the nervous system and the skin.
IP affects the skin, eyes, hair, teeth, nails, and the central nervous system, which includes the brain and spinal cord. Skin problems are the most common symptom of IP and tend to be apparent at birth or within two weeks of birth. People with IP may also have severe vision loss, cataracts, or crossed eyes; missing or peg-shaped teeth; and poorly developed hair and nails.
Neurological problems in IP include wasting away of the brain tissue, formation of small holes in the brain tissue, and the loss of nerve cells. Additional symptoms of IP include intellectual disabilities, seizures, muscle weakness in one or both sides of the body, and slow motor development.
IP is caused by a mutation in the NEMO gene (also known as IKBKG). The NEMO gene provides instructions for making the NEMO protein, which is important for the immune system and for the health of cells. NEMO is also involved with the development of the skin, eyes, teeth, and hair.
People with IP may be at higher risk for certain types of cancer, such as leukemia, because of instability in the chromosomes. Although the skin abnormalities usually become less apparent and sometimes disappear completely, there may be residual neurological difficulties.
The incidence of incontinentia pigmenti is one in 40,000 individuals worldwide, and it is more common in Caucasians than in other races. Incontinentia pigmenti usually affects only females, because it is an X-linked dominant disease; male fetuses usually do not survive.
Risk Factors
Because incontinentia pigmenti (IP) is typically a genetic disorder, the only known risk factor is a family history of the condition.
X-linked inheritance: IP is inherited, or passed down among family members, according to an X-linked dominant pattern. Females have two copies of the X chromosome and males have one copy of the X and one copy of the Y chromosome. Because IP is a dominant trait, only one copy of the mutated gene is necessary for the condition to occur. Because IP is an X-linked condition, individuals can inherit it only from their mothers.
IP is very rare, occurring in about one in 40,000 people. There are only about 700-1,000 known cases in the scientific literature. It is more common among Caucasians than among people of other races. IP tends to affect more females than males. Male fetuses with IP usually die before birth. This is because they inherit only one copy of the X chromosome, which turns out to be fatal for this disease.
Random occurrence: In about half of all cases of IP, there is no family history of the condition. In these cases, the disease is caused by a spontaneous mutation in the egg, sperm cell, or developing fetus. The risk factors for random occurrence are not known.
Other: Infections also seem to play a role in the reoccurrence of IP. Researchers have reported that infections may trigger the NEMO gene to cause the reoccurrence of previous pigmentations after a period where the NEMO gene was thought to be dormant.
Causes
Incontinentia pigmenti (IP) is caused by a mutation in the NEMO gene (also known as IKBKG). The NEMO gene provides instructions for making the NEMO protein, which is important for the immune system and for the health of cells. NEMO is also involved in the development of the skin, eyes, teeth, and hair.
The NEMO gene (an NF-kappaB essential modulator) is located on the X chromosome and is essential to the activation of the NF-kappaB transcription factor, which participates in many immune, inflammatory, and apoptotic (cell death) pathways. Different NEMO gene mutations have been identified. Approximately 80% of IP patients have been shown to carry a common deletion mutation that removes some protein-encoding regions of the NEMO gene.
The NEMO gene provides instructions for making a protein that helps regulate the activity of nuclear factor-kappaB. Nuclear factor-kappaB is a protein complex important for cell survival, and if it is not properly regulated, cells will die. In about 80% of affected individuals, mutations in the IKBKG gene lead to an abnormally small, nonfunctional version of the IKBKG protein. Other people with IP have mutations that prevent any production of the IKBKG protein. Researchers believe that abnormal cell death caused by inadequate amounts of this key protein leads to the signs and symptoms of IP.
Signs and Symptoms
Cognitive: Patients with incontinentia pigmenti (IP) may have varying degrees of intellectual disability. They may also have behavioral problems.
Dental: People with IP may have absent, small, or misshapen teeth. Teeth may also be slow to develop, be especially vulnerable to cavities, and have weak enamel.
Eyes: Vision problems are common in IP. These may include vision loss (ranging from mild to severe), cataracts, and crossed eyes. Other problems may include changes in eye pigments, abnormal blood vessels in the eye, small eyes, glaucoma, and retinal detachment.
Hair: In IP, the hair is typically thin, woolly, and poorly developed. There may also be bald patches.
Muscular: Patients with IP have slow motor development. Muscle weakness on one or both sides of the body may be apparent. Coordination problems and problems with mobility may also occur.
Nails: Poorly developed nails are a common feature of IP, occurring in about 40-60% of patients. Small tumors may also develop under the nails.
Neurological: Neurological problems include wasting of the brain tissue, formation of small holes in the brain tissue, loss of nerve cells, and seizures. Additional symptoms may include a small brain and vulnerability to strokes and a brain disease known as encephalopathy.
Skeletal: In a few cases, skeletal problems occur with IP. These may include scoliosis (curvature of the spine), extra ribs, and skull deformities.
Skin: The most common and often the earliest symptom of IP is discoloration of the skin. This is caused when melanin, which gives normal skin its color or pigment, collects in the skin, causing wavy lines and streaks that are gray, blue, or brown.
Skin symptoms of IP may occur in four stages. In stage 1, skin problems look like pimples or blisters. These are often present at birth, are common along the torso, and may recede with time. However, illness and other stressors may cause them to reappear. Stage 2, which occurs between two and eight weeks of age, is marked by wartlike growths. In stage 3, between ages 12 and 40 weeks, the skin develops wavy streaks that follow a pattern known as Blaschko lines. In stage 4, the amount of pigment decreases and the streaks appear lighter than the rest of the skin.
Other: In rare cases, patients with IP may develop heart failure and high blood pressure in the pulmonary artery, or the artery leading to the lungs. This condition is pulmonary hypertension.
Diagnosis
Physical exam: Diagnosis of incontinentia pigmenti (IP) is made after completing a thorough family history and a complete physical exam. A clinician will look for the distinctive features of IP in the skin, eyes, hair, teeth, and nails. Discolored skin is caused by excessive deposits of melanin (normal skin pigment), especially in the trunk and extremities. Discolored skin is slate-gray, blue, or brown and is distributed in irregular, marbled or wavy lines. The discoloration fades with age. Neurological problems include cerebral atrophy, the formation of small cavities in the central white matter of the brain, and loss of neurons in the cerebellar cortex, which is the region of the brain that controls movement and coordination. About 20% of children with IP will have slow motor development, muscle weakness in one or both sides of the body, intellectual disabilities, and seizures. They are also likely to have vision problems, including crossed eyes, cataracts, and severe vision loss. Dental problems are also common, including missing or peg-shaped teeth.
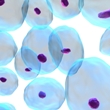
Biopsy: In a biopsy, a small sample of tissue is taken and examined under a microscope. To confirm a diagnosis of IP, a clinician may take a skin biopsy to check for distinctive types of cells, such as eosinophils (white blood cells) in the dermis and epidermis.
Imaging: Computed tomography (CT) or magnetic resonance imaging (MRI) may be used to determine the presence, type, and degree of brain disease. Imaging studies can also be used to determine the health of blood vessels in the eye.
Genetic (DNA) testing: Deoxyribonucleic acid (DNA) tests may also be performed to confirm the presence of the mutated NEMO gene that causes IP and to confirm the results from other tests.
Amniotic fluid (prenatal) genetic testing: Genetic tests may also be performed on blood from a developing fetus or amniotic fluid, which is the fluid contained in the sac that surrounds and cushions the fetus. Because taking a blood sample may cause harm to a fetus, taking samples of amniotic fluid is generally preferred. It is important to note that any prenatal test carries a risk of miscarriage.
Chorionic villus sampling (CVS): Chorionic villus sampling (CVS) is another type of prenatal diagnosis that can detect genetic problems in a fetus. Samples are taken of the chorionic villi, or placental tissue. As with any prenatal test, this procedure carries a risk of miscarriage.
Preimplantation genetic diagnosis (PGD): A new procedure called preimplantation genetic diagnosis (PGD) may be performed on embryos produced by in vitro (artificial) fertilization. This test allows parents to implant and carry only the embryos that do not have the mutated genes that cause IP.
Complications
Cancer: People with incontinentia pigmenti (IP) may be at an increased risk for certain cancers, including acute myelogenous leukemia, which is a cancer of the white blood cells; Wilms tumor, a tumor of the kidneys; malignant rhabdoid tumor of the kidney, a variant of Wilms tumor; and retinoblastoma, a cancer that affects the retina.
Coordination and development: Because of abnormalities in the cerebellum, people with IP often have ataxia (problems with balance and coordination). People with IP may also have delayed development of overall motor and speech skills. Problems with coordination and development depend on how severely the brain is affected in this condition.
Dental: People with IP may have absent, small, or misshapen teeth. Teeth may also be slow to develop, be especially vulnerable to cavities, and have weak enamel.
Neurological: Neurological problems include wasting of the brain tissue, formation of small holes in the brain tissue, loss of nerve cells, and seizures. Additional symptoms may include a small brain and vulnerability to strokes and a brain disease known as encephalopathy.
Treatment
General: There is no treatment for incontinentia pigmenti (IP). Instead, treatment aims to manage symptoms and prevent complications.
Dental care: Patients with IP require regular dental care, including brushing teeth after meals or at least twice daily. Patients with IP should have regular follow-up visits with a dentist. Orthodontic treatment may be recommended to straighten teeth if they are not aligned properly.
Eye care: Vision loss may be improved with corrective lenses, drugs, or even surgery in severe cases. Patients should be seen by an ophthalmologist as soon as possible following birth, monthly until three to four months of age, every three months until one year of age, twice yearly until three years of age, and yearly thereafter.
Neurological: Patients who have seizures, muscle spasms, or paralysis may be treated with drugs or medical devices. If neurological symptoms such as seizures are present, patients with IP should have regular follow-up visits with a neurologist.
Skin care: While skin abnormalities are usually the first apparent symptom of IP, they tend to fade by adolescence or adulthood. Patients may choose to use makeup to hide the abnormal coloration.
Integrative Therapies
Currently, there is limited scientific evidence on the use of integrative therapies for the treatment or prevention of incontinentia pigmenti (IP).
Prevention
General: Because incontinentia pigmenti (IP) is an inherited condition, there is no known way to prevent the disease. However, a number of options are available for prospective parents with a family history of IP.
Genetic testing and counseling: Individuals who have IP may meet with a genetic counselor to discuss the risks of having children with the disease.
Genetic counselors can explain the options and the associated risks of various tests, including preimplantation genetic diagnosis (PGD), amniocentesis, and chorionic villus sampling (CVS).
Preimplantation genetic diagnosis (PGD) may be used with in vitro (artificial) fertilization. In PGD, embryos are tested for the genes that cause IP, and only the embryos that are free of those mutations may be selected for implantation. Because IP can be detected in a fetus, parents may choose whether to continue the pregnancy. Genetic counselors may assist parents with these difficult decisions.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Ardelean D, Pope E. Incontinentia pigmenti in boys: a series and review of the literature. Pediatr Dermatol. 2006;23(6):523-7. View Abstract
Carney RG. Incontinentia pigmenti. A world statistical analysis. Arch Dermatol. 1976;112(4):535-42. View Abstract
Ciarallo L, Paller AS. Two cases of incontinentia pigmenti simulating child abuse. Pediatrics. 1997;100(4):E6. View Abstract
Ectodermal Dysplasia Society. www.ectodermaldysplasia.org.
Hadj-Rabia S, Froidevaux D, Bodak N, et al. Clinical study of 40 cases of incontinentia pigmenti. Arch Dermatol. 2003;139(9):1163-70. View Abstract
Happle R. Incontinentia pigmenti versus hypomelanosis of Ito: the whys and wherefores of a confusing issue. Am J Med Genet. 1998;79(1):64-5. View Abstract
Happle R. A fresh look at incontinentia pigmenti. Arch Dermatol. 2003;139(9):1206-8. View Abstract
Jandeck C, Kellner U, Foerster MH. Successful treatment of severe retinal vascular abnormalities in incontinentia pigmenti. Retina. 2004;24(4):631-3. View Abstract
Kasmann-Kellner B, Jurin-Bunte B, Ruprecht KW. Incontinentia pigmenti (Bloch-Sulzberger-syndrome): case report and differential diagnosis to related dermato-ocular syndromes. Ophthalmologica. 1999;213(1):63-9. View Abstract
Minic S, Novotny GE, Trpinac D, et al. Clinical features of incontinentia pigmenti with emphasis on oral and dental abnormalities. Clin Oral Investig. 2006;10(4):343-7. View Abstract
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Pacheco TR, Levy M, Collyer JC. Incontinentia pigmenti in male patients. J Am Acad Dermatol. 2006;55(2):251-5. View Abstract
Phan TA, Wargon O, Turner AM. Incontinentia pigmenti case series: clinical spectrum of incontinentia pigmenti in 53 female patients and their relatives. Clin Exp Dermatol. 2005;30(5):474-80. View Abstract
Woffendin H, Jakins T, Jouet M, et al. X-inactivation and marker studies in three families with incontinentia pigmenti: implications for counselling and gene localisation. Clin Genet. 1999;55(1):55-60. View Abstract
Wong GA, Willoughby CE, Parslew R. The importance of screening for sight-threatening retinopathy in incontinentia pigmenti. Pediatr Dermatol. 2004;21(3):242-5. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017