Hypomelanosis of Ito
Hypomelanosis of Ito
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
HMI, incontinentia pigmenti achromians, incontinentia pigmenti type 1 (formerly), IP1 (formerly), IPA, ITO, ITO hypomelanosis, sporadic incontinentia pigmenti.
Background
Hypomelanosis of Ito (HI) syndrome is one of several ectodermal dysplasias, a group of syndromes deriving from abnormalities of the ectodermal structures, which include the hair, teeth, nails, sweat glands, cranial-facial structure, and hands. HI is a genetic condition, but it is unclear whether it may be inherited.
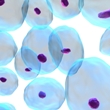
A distinctive feature of HI is hypopigmentation, or the lack of the pigment melanin, which gives color to the skin and hair. Hypopigmentation affects many parts of the body, and in HI it takes on a pattern known as the "lines of Blaschko." The cause of this pattern is unknown, and it does not correspond to any particular anatomical feature.
HI is marked by a lack of skin pigment on many parts of the body. The absence of pigment in skin may appear as streaks, patches, and whorls and may follow the Blaschko lines pattern. Individuals with HI may have intellectual and developmental disabilities, seizures, and other nerve disorders. Other physical characteristics of HI include a small head and problems with the skeleton, eyes, and teeth.
HI (previously known as IP type 1 or IP1) is a rare genetic disorder similar to incontinentia pigmenti (IP), which is also known as IP type 2 or IP2. However, HI has additional features, and some argue that these make HI a distinct condition. Many people describe HI as being like a negative image of IP, which is characterized by discolored skin caused by excessive deposits of melanin. In IP, melanin collects in the skin, causing wavy lines and streaks that are gray, blue, or brown.
HI is a genetic condition, but it is unclear whether it may be inherited. There are several candidate genes that may contribute to the disease, but no consensus has been reached about the genetic basis or inheritance pattern of this disease.
HI is extremely rare. It does not seem to occur in any population more frequently than another, although it affects slightly more females than males.
HI may present in many different ways in different individuals. People in whom HI symptoms are limited to the skin tend to have a normal lifespan. The severity of neurological symptoms often determines health status and quality of life. Death from HI is rare.
Risk Factors
Because hypomelanosis of Ito (HI) syndrome is typically a genetic disorder, the only known risk factor is a family history of the condition.
In recent studies, the male-to-female ratio of HI was 1:1.2, meaning that females may be slightly more affected by HI than males. The symptoms and the severity of symptoms are similar in males and females. HI does not appear to affect any other specific population more than another.
Causes
Although a wide range of sporadic chromosomal abnormalities may be observed, researchers believe that regions on chromosome 9, 15, and X [9q33-ter, 15q11-q13, Xp11], may be involved in hypomelanosis of Ito (HI) syndrome. These letters and numbers refer to the location of the abnormalities on the gene. Autosomal deletions and duplications may involve chromosomes 7, 12, 13, 14, 15, and 18. Many patients have a chromosomal mosaic pattern, which occurs when a person's cells do not have the same chromosome composition. This pattern can lead to the generation of two cell lineages that produce patterns of hypopigmented and hyperpigmented skin. X chromosome alterations are not unusual in HI. Recent evidence points to X chromosome inactivation, activation, and mosaicism as the main causes of these different patterns of cell behavior in the skin.
HI is a genetic condition, but it is unclear whether it may be inherited. There are several candidate genes that may contribute to the disease, but no consensus has been reached about the genetic basis or inheritance pattern of this disease. Research in these areas is conflicting.
There is a lack of supporting evidence to suggest that HI can occur through a spontaneous mutation.
Signs and Symptoms
General: Hypomelanosis of Ito (HI) syndrome may involve many organs. Several signs, such as seizures and mental retardation, may be found in the individual's medical history. The skin and neurological signs and symptoms are primary to a diagnosis of HI. The involvement of other organ systems is secondary but should still be considered. A distinctive feature of HI is hypopigmentation, or the lack of the pigment melanin that gives color to the skin and hair. Hypopigmentation affects many parts of the body, and in HI it may take on a pattern known as the "lines of Blaschko." The cause of the lines of Blaschko is unknown, and this pattern does not correspond to any particular anatomical feature.
Dental: People with HI may have absent, small, or misshapen teeth. Teeth may also be slow to develop, be especially vulnerable to cavities, and have weak enamel.
Developmental problems: Individuals with HI often have intellectual and other developmental disabilities. Intellectual disability is seen in about 60% of patients with HI. Autism is seen in about 10% of these patients.
Nails: Poorly developed nails are a common feature of HI, occurring in about 40-60% of patients. Small tumors may also develop under the nails.
Nervous system: The nervous system may be affected in patients with HI. Neurological problems can range from mild to severe. Epilepsy is seen in about 50% of people with this disorder.
Skin: The most common symptom of HI is the absence of color or pigment in the skin. This absence may appear in whorls, streaks, or patches and tends to follow a pattern known as the "lines of Blaschko." The cause of the lines of Blaschko is unknown, and this pattern does not correspond to any particular anatomical feature.
Vision: Individuals with HI may present with various eye problems, including cataracts (a clouding of the lens of the eye) or a breakdown of the cells in the retina (back of the eye), which is present in approximately one-fifth of patients. A loss of vision may occur. Other problems may include changes in eye pigment, abnormal blood vessels in the eye, small eyes, and glaucoma.
Other: People with HI may also have a small head and problems with the eyes, teeth, and skeleton. In addition, one side of the body may appear to develop faster than the other. In rare cases, heart, digestive, or kidney problems occur.
Types of the Disease
A familial form of hypomelanosis of Ito (HI) syndrome exists. However, fewer than 3% of the patients have a family history of HI-type skin lesions.
There is a lack of evidence to suggest that HI always occurs through a spontaneous mutation. Some researchers suggest that the abnormalities causing HI may occur after fertilization and for unknown reasons. However, research in this area is conflicting.
Diagnosis
General: The symptoms of hypomelanosis of Ito (HI) syndrome generally appear by the time a child is two years of age.
Physical exam: Diagnosis of HI may begin with a thorough family history and complete physical exam. The clinician may ask about a history of seizures, intellectual disabilities, and developmental delays. He or she may check for distinctive skin problems, which include hypopigmented areas of skin that appear as streaks, whorls, or patches that may be located on just one side of the body or on both sides; hair problems, which include slow growth, white hair, or increased facial hair; vision problems, such as cataracts (a clouding that develops on the lens of the eye) or a breakdown of the cells in the retina (back of the eye), which is present in approximately one-fifth of HI patients; and tooth and mouth problems, including teeth that are not properly aligned or have defective tooth enamel. Referrals may be made to assess the type and degree of vision problems and intellectual or developmental disabilities.
Imaging: If neurological symptoms are apparent, imaging studies can help clinicians understand the degree of severity and the specific type of disorder. Computed tomography (CT), magnetic resonance imaging (MRI), and electroencephalograms (EEG) may be used. Radiographs may also be used to assess bone problems. Electromyelography (EMG) can assess whether there is decreased muscle tone.
Neurological exam: Patients should receive a neurological exam to assess the extent of neurological problems, including seizures and psychomotor delays.
Genetic (DNA) testing: Testing may also be performed to confirm the presence of chromosomal abnormalities, but since the gene responsible for HI is unknown, DNA tests cannot be used to diagnose HI.
Complications
Complications associated with hypomelanosis of Ito (HI) syndrome are related to the severity of neurological problems. In the most severely affected individuals, seizures may place them at increased risk of brain injury.
Treatment
General: There is no cure for hypomelanosis of Ito (HI) syndrome. Instead, treatment aims to relieve symptoms and prevent complications. There are no available treatments for the absence of pigment in the skin. Patients may choose to wear makeup to cover colorless spots. Patients with HI may consult with neurologists, psychiatrists, orthopedists, dentists, and ophthalmologists depending of the presence and severity of symptoms.
Depending on the level of intellectual and developmental disabilities, some patients may be able to live independently once they reach adulthood, while others may need lifelong support and residential care. Adults with profound intellectual disabilities usually require lifelong nursing care.
Behavioral therapy: Behavioral therapy may also be beneficial. Several different types of behavioral therapy are available to help patients improve their communication and social skills and maximize their learning abilities and adaptive behaviors. Evidence suggests that behavioral therapy is most effective when it is started early in life (3-4 years of age or younger).
Dental care: Patients with HI require regular dental care, including brushing teeth after meals or at least twice daily. Patients with HI should have regular follow-up visits with a dentist. Orthodontic treatment may be recommended to help straighten the teeth if they are not aligned properly.
Drug therapy: Based on the severity of symptoms, a clinician may choose to use drug therapy to control the seizures seen in HI-related epilepsy.
Education: By law, patients with HI must have access to education that is tailored to their specific strengths and weaknesses. According to the Individuals with Disabilities Education Act, all children with disabilities must receive free and appropriate education. According to the law, staff members of the patient's school should consult with the patient's parents or caregivers to design and write an individualized education plan. The school faculty must document the child's progress in order to ensure that the child's needs are being met.
Educational programs vary among patients. In general, most experts believe that children with disabilities should be educated alongside their nondisabled peers. The idea is that nondisabled students will help the patient learn appropriate behavioral, social, and language skills. Therefore, some patients with intellectual disabilities are educated in mainstream classrooms. Others attend public schools but take special education classes, and still others attend specialized schools that are equipped to teach children with disabilities.
Eye care: Vision loss may be improved with corrective lenses, drugs, or even surgery in severe cases. Patients should be seen by an ophthalmologist as soon as possible following birth, monthly until three to four months of age, every three months until one year of age, twice yearly until three years of age, and yearly thereafter.
Neurological: Patients with HI who have seizures, muscle spasms, or paralysis may be treated with drugs and medical devices. If neurological symptoms such as seizures are present, patients should have regular follow-up visits with a neurologist.
Occupational therapy: Patients may benefit from occupational therapy. During sessions, a therapist helps the child learn skills needed to perform basic daily tasks, such as eating, dressing, and communicating with others. Parents and caregivers can ask their child's pediatrician for recommended therapists.
Speech-language therapy: Some patients with HI may benefit from speech-language therapy because they often develop communication skills more slowly than normal. During speech-language therapy, a qualified speech-language professional (SLP) works with the patient on a one-to-one basis, in a small group, or in a classroom to help the patient improve speech, language, and communication skills. Programs are tailored to the patient's individual needs.
Speech pathologists use a variety of exercises to improve the patient's communication skills. Exercises typically start simple and become more complex as therapy continues. For instance, the therapist may ask the patient to name objects, tell stories, or explain the purpose of an object.
On average, patients receive five or more hours of therapy per week for three months to several years. Doctors typically recommend that treatment be started early to ensure the best possible outcome for the child.
Integrative Therapies
Currently there is a lack of scientific evidence on the use of integrative therapies for the treatment or prevention of hypomelanosis of Ito (HI) syndrome.
Prevention
General: Although hypomelanosis of Ito (HI) syndrome is thought to be a genetic condition, there is a lack of evidence to support spontaneous mutation. Some researchers suggest that the abnormalities causing HI may occur after fertilization and for unknown reasons. However, research in this area is conflicting. A familial form of HI exists, but fewer than 3% of patients have a family history of HI-type skin lesions.
Genetic testing and counseling: Individuals who have HI may meet with a genetic counselor to discuss the risks of having children with the disease.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Bitoun P, Philippe C, Cherif M, et al. Incontinentia pigmenti (type 1) and X;5 translocation. Ann Genet. 1992;35: 51-4. View Abstract
Browne RM, Byrne JPH. Dental dysplasia in incontinentia pigmenti achromians (Ito): an unusual form. Brit Dent J. 1976;140: 211-4. View Abstract
Crolla JA, Gilgenkrantz S, de Grouchy J, et al. Incontinentia pigmenti and X-autosome translocations: non-isotopic in situ hybridization with an X-centromere-specific probe (pSV2X5) reveals a possible X-centromeric breakpoint in one of five published cases. Hum Genet. 1989;81:269-72. View Abstract
Donnai D, Read AP, McKeown C, et al. Hypomelanosis of Ito: a manifestation of mosaicism or chimerism. J Med Genet. 1988;25:809-18. View Abstract
Ectodermal Dysplasia Society. www.ectodermaldysplasia.org.
Flannery DB. Pigmentary dysplasias, hypomelanosis of Ito, and genetic mosaicism. (Editorial) Am J Med Genet. 1990;35:18-21. View Abstract
Genetics Home Reference. http://ghr.nlm.nih.gov.
Glover MT, Brett EM, Atherton DJ. Hypomelanosis of Ito: spectrum of the disease. J Pediatr. 1989;115(1):75-80. View Abstract
Grosshans EM, Stoebner P, Bergoend H, et al. Incontinentia pigmenti achromians (Ito). Dermatologica 1971;142: 65-78. View Abstract
Happle R. Incontinentia pigmenti versus hypomelanosis of Ito: the whys and wherefores of a confusing issue. Am J Med Genet. 1998;79: 64-5. View Abstract
Hatchwell E. Hypomelanosis of Ito and X; autosome translocations: a unifying hypothesis. J Med Genet. 1996;33(3):177-83. View Abstract
Koiffmann CP, de Souza DH, Diament A et al. Incontinentia pigmenti achromians (hypomelanosis of ITO, MIM 146150): further evidence of localization at Xp11. Am J Med Genet. 1993;46: 529-33. View Abstract
Montagna P; Procaccianti G; Galli G; et al. Familial hypomelanosis of Ito. Eur Neurol. 1991;31: 345-7. View Abstract
Moss C, Burn J. Genetic counselling in hypomelanosis of Ito: case report and review. Clin Genet. 1988;34:109-15. View Abstract
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Pascual-Castroviejo I, Roche C, Martinez-Bermejo A, et al. Hypomelanosis of ITO. A study of 76 infantile cases. Brain Dev. 1998;20(1):36-43. View Abstract
Rutland B, Edgar M, Horenstein M. Hypomelanosis of Ito associated with precocious puberty. Pediatric Neurology. 2006;34(1):51-4. View Abstract
Urgelles E, Pascual-Castroviejo I, Roche C, et al. Arteriovenous malformation in hypomelanosis of Ito. Brain Dev. 1996;18:78-80. View Abstract
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017