Fungal infections
Fungal infections
Natural Standard Monograph, Copyright © 2013 (www.naturalstandard.com). Commercial distribution prohibited. This monograph is intended for informational purposes only, and should not be interpreted as specific medical advice. You should consult with a qualified healthcare provider before making decisions about therapies and/or health conditions.
Related Terms
Antifungal, athlete's foot, Candida albicans, dermatophytes, fingernail infection, fungal infection, fungal nail infection, fungal scalp infection, fungal spores, fungi, fungus, histoplasmosis, jock itch, molluscum contagiosum, mucocutaneous candidiasis, nail infections, onychomycosis, oral candidiasis, oral thrush, paronychia, thrush, tinea capitis, tinea cruris, tinea pedis, tinea versicolor, toenail infection, yeast infection.
Background
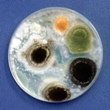
Some organisms, called fungi, may cause diseases in humans. When a fungus's tiny reproductive cells (spores) enter the body or come into contact with the skin and begin to multiply, it is called a fungal infection.
Fungi may be found in virtually every type of habitat including land, fresh water, and salt water. However, they are most common in dark, moist, and warm environments. They are often found in the soil, on food, and on the skin.
Most types of fungi are harmless to humans.
Disease-causing fungi may enter the body through the skin, nose, vagina, nails, or mouth. This is because these areas of the body are the most likely to be exposed to fungi.
Fungi cause different diseases depending on the specific type of fungus and where they are in the body. Examples of common fungal infections include athlete's foot, candidiasis, histoplasmosis, jock itch (tinea cruris), onychomycosis, fungal paronychia, tinea capitis, and tinea versicolor.
Most fungal infections do not cause serious medical problems. If left untreated, some types of fungal infections may spread to other parts of the body and even lead to death. However, if diagnosed and treated quickly, most patients with fungal infections experience a complete recovery. Fungal infections are treated with medications called antifungals. Depending on the type, severity, and location of the infection, as well as the patient's overall health, antifungals may be taken by mouth, applied to the skin, or injected into the vein.
Common Types and Causes of Fungal Infections
Athlete's foot (tinea pedis): Athlete's foot (tinea pedis) is a fungal infection of the foot that causes itching, stinging, and burning.
A group of fungi, called dermatophytes, cause athlete's foot. These fungi prefer warm moist environments. Individuals whose feet are exposed to this type of environment have an increased risk of developing an infection. Patients may be exposed to the fungi when they shower barefoot in a public facility, such as a gym.
Once the fungus comes into contact with human skin, it begins to reproduce. As a result, the top layer of the skin produces more skin cells than normal. This causes the skin on the feet to become thick, scaly, and itchy.
Most cases of athlete's foot can be treated with over-the-counter (OTC) antifungal medications. More severe infections that do not respond to OTC treatment may require prescription-strength antifungals.
Candidiasis: Mucocutaneous candidiasis is an opportunistic infection caused by the fungus Candida albicans. Opportunistic infections occur in individuals who have weakened immune systems. The infection can affect the mouth (oral candidiasis or oral thrush), esophagus (esophageal candidiasis), or vagina (vulvovaginal candidiasis or yeast infection).
The Candida albicans fungus is found almost everywhere in the environment, which is why most people have small amounts of Candida albicans in their mouth and/or vagina at any given time. However, individuals with healthy immune systems are usually able to prevent the fungus from multiplying and causing an infection. In rare cases, when candidiasis affects healthy individuals, symptoms are usually minor. In contrast, immunocompromised patients, such as HIV patients or patients receiving immunosuppressants, often suffer from severe symptoms including painful lesions in the mouth that make it difficult to eat.
In addition to pathogenic bacteria in the body, antibiotics may also eliminate normal, healthy bacteria which may allow for the overgrowth of Candida. Use of oral antibiotics, especially broad spectrum antibiotics, has been associated with an increased occurrence of yeast infection. Antibiotics have also been detected in animal products such as meat, poultry, and cow's milk. In human study, significantly higher Candida albicans counts were found in the stool of patients with antibiotic-associated diarrhea (AAD).
If left untreated, oral candidiasis may progress to esophageal candidiasis, which occurs when the infection spreads to the esophagus. The esophagus is the tube that leads from the mouth to the stomach. Drugs that suppress acid production, such as H2-blockers and proton pump inhibitors, may contribute to fungal infections of the upper gastrointestinal tract and may predispose some patients to infectious Candida esophagitis.
Vaginal candidiasis (yeast infection) is common in both healthy and immunocompromised patients. Researchers estimate that about 75% of all women are likely to have at least one vaginal Candida infection during their lifetime and up to 45% experience two or more. Individuals who become pregnant, take high-estrogen birth control pills, have uncontrolled diabetes mellitus, wear tight-fitting clothes, receive antibiotic therapy, or have sexually transmitted diseases have an increased risk of developing yeast infections.
Candidiasis infections are generally treated with antifungals. Treatment generally lasts about 10 to 14 days.
Histoplasmosis: Histoplasmosis is a fungal infection of the lungs that may spread to other organs and tissues of the body.
The Histoplasma capsulatum fungus causes histoplasmosis. The fungus is commonly found in damp soil that is rich in organic material. The tiny reproductive cells of the fungus (spores) enter the body through the nose or mouth when a patient inhales or consumes contaminated food or water.
Most patients with histoplasmosis do not experience any symptoms of the disease and do not require treatment. This is because healthy individuals have strong immune systems that are able to prevent the fungi from multiplying and causing an infection.
However, patients with weakened immune systems, especially HIV patients and infants, are vulnerable to developing infections that start in the lungs and spread to other areas of the body. When the infection spreads, it is called disseminated histoplasmosis. This condition is fatal if left untreated.
Patients with underlying diseases, such as emphysema, are also vulnerable to developing a long-term infection that primarily affects the lungs. When this happens, the condition is called chronic pulmonary histoplasmosis. Patients with this type of infection require lifelong treatment with antifungals.
In some cases, otherwise healthy individuals may develop histoplasmosis infections. This may happen if the patient is exposed to large amounts of the fungus. For instance, farmers who are frequently exposed to soil or bird or bat droppings have an increased risk of developing infections.
Jock itch (tinea cruris): Jock itch, also called tinea cruris, is a fungal infection that affects the skin of the inner thighs, buttocks, and genitals.
Jock itch is caused by a group of fungi called dermatophytes. The fungi that cause jock itch are usually the same organisms that causes athlete's foot, tinea capitis (ringworm of the scalp), and tinea versicolor. These organisms normally live on the skin and do not cause an infection. However, when areas of the body are frequently moist, the fungi may grow uncontrollably. Although anyone can acquire the infection, it is most common in individuals who sweat a lot, such as athletes or those who are overweight. This is because a warm and sweaty environment provides an especially good habitat for fungi.
Jock itch is mildly contagious. It may spread through physical contact or after using shared items (e.g. towels) that came into contact with the infected person's skin.
Jock itch is not a serious infection. It is usually treated with antifungals that are applied to the skin.
Onychomycosis: Onychomycosis is a fungal infection of the nail bed.
A group of fungi called dermatophytes are usually the cause of onychomycosis. The fungi that cause the infection prefer warm moist environments. Therefore, patients are most likely to develop onychomycosis if their nails are frequently exposed to such environments, such as sweaty socks or shower floors. Toenails are more likely to be affected than fingernails.
Onychomycosis can be successfully treated with oral antifungals.
Fungal paronychia: Fungal paronychia is a fungal skin infection that occurs near the nail beds. It causes the skin around the fingernails or toenails to become red and swollen. It may also cause pus-filled blisters to form.
Fungal paronychia is commonly caused by a group of fungi called dermatophytes. Fungal paronychia is common among patients with onychomycosis, diabetes, and those who are frequently getting their hands wet for long periods of time (e.g. swimmers). Biting the nails, hangnails, or pushing back the cuticles also increases the risk of an infection.
Patients respond well to treatment with antifungals. However, it may take several months for the infection to be completely cured.
Tinea capitis (ringworm of the scalp): Tinea capitis, also called ringworm of the scalp, is a fungal infection of the skin on the head.
Tinea capitis is caused by a group of fungi called dermatophytes. Once the disease-causing fungi come into contact with the skin, the organism begins to multiply and an infection develops. Tinea capitis is contagious, and it can spread through skin-to-skin contact. Patients may be exposed to the fungi after touching an infected animal, such as a dog, cat, ferret, rabbit, goat, or pig. Patients may also become infected after touching objects (e.g. towels, clothing, or bed linens) that an infected person or animal has been in contact with.
Tinea versicolor: Tinea versicolor is a common fungal infection of the skin that causes patches of the skin to appear lighter than normal. The infection generally worsens during hot and humid weather.
Tinea versicolor is caused by Malassezia furfur, which is normally found on the skin. Many factors, including hot and humid weather, immunosuppression, hormonal changes, excessive sweating, or oily skin, may trigger the fungi to multiply uncontrollably and cause an infection.
It may take several weeks for antifungal cream and lotions to completely eliminate the fungus from the body.
Signs and Symptoms
General: Symptoms vary depending on the type and severity of the infection, as well as the parts of the body that are infected. Patients should visit their healthcare professionals if any of these symptoms develop.
Nail beds: Patients who have fungal nail infections (onychomycosis) may develop thick, brittle, or crumbly fingernails or toenails, which may be painful. The nails may become distorted in shape, flat, or dull. The nails may be yellow, green, brown, or black in color, and they may emit a foul odor. In some cases, infected nails may separate from the nail bed, causing a condition called onycholysis.
Scalp: Patients with fungal infections of the scalp (e.g. tinea capitis) typically develop a circle-shaped rash on the skin that is swollen. The skin may be scaly and itchy. There may be small black dots on the scalp. Patients may lose small patches of hair. However, the hair will grow back once treatment is started.
Skin: Symptoms of tinea versicolor, which is the most common type of fungal skin infection, typically include patches of discolored skin that grow slowly and prevent the skin from tanning. As a result, symptoms are usually most apparent after the skin is exposed to the sun. The patches of scaly skin may be various colors, such as white, pink, tan, or dark brown. The affected skin may also be itchy. The back, chest, neck, and upper arms are most likely to be affected. Symptoms may worsen during hot and humid weather.
Mouth: Symptoms of oral thrush may develop suddenly. Oral thrush typically causes creamy white lesions on the tongue, inner cheek, and sometimes, the gums, tonsils, and roof of the mouth. These lesions are often painful in patients with weakened immune systems, and they may bleed slightly when they are rubbed.
Esophagus: Severe cases of oral thrush may spread into the esophagus. This is most likely to occur if oral thrush is left untreated or if the patient is extremely immunocompromised. Common symptoms of esophageal candidiasis include pain or difficulty swallowing and the sensation of food sticking to the throat. The pain may be so severe that it is difficult to eat. A fever may indicate that the infection has spread beyond the esophagus.
Lungs: Symptoms of histoplasmosis typically develop about 17 days after the fungal spores were inhaled. Common symptoms include fever, headache, dry cough, chills, chest pain, weight loss, and sweats.
Vagina: Common symptoms of vulvovaginal candidiasis (yeast infection) include itching, watery or curd-like vaginal discharge that is white in color, vaginal erythema (reddening of the skin), pain during sexual intercourse (dyspareunia), painful urination, swollen labia and vulva, and vaginal lesions. Symptoms generally worsen during menstruation because the hormonal changes provide a better environment for fungal growth.
Feet: Fungal infections of the feet, such as athlete's foot, may cause burning or itching anywhere on the feet. Symptoms are usually most noticeable in between the toes. Patients may also develop itchy blisters, cracked or peeling skin, dry skin, or toenails that are thick, crumbly, discolored, or pulling away from the nail bed.
Systemic: When a fungal infection enters the bloodstream and affects multiple body tissues and organs, the condition is often life threatening. Histoplasmosis may spread to virtually any part of the body, including the liver, bone marrow, eyes, skin, adrenal glands, and/or intestinal tract. When this happens, the condition is called disseminated histoplasmosis. Symptoms vary depending on which organs are infected. It may lead to severe and fatal complications, including pneumonia, pericarditis, meningitis, and/or adrenal insufficiency.
If left untreated, a severe candidiasis infection may spread into the bloodstream and affect other organs, including the intestines, kidneys, or heart. This condition is called candidemia. Fever and low blood pressure often occur in patients with candidemia. Additional symptoms depend on which body parts are affected. For instance, if the heart becomes infected, it may cause a heart murmur or enlargement of the spleen.
Diagnosis
Most fungal infections are diagnosed after the fungi are identified in the patient's blood or tissue. The healthcare provider will take a small sample of tissue from the affected area. For instance, if the patient's symptoms involve the respiratory tract, a healthcare provider may swab the back of the patient's throat. The sample is then analyzed under a microscope for the presence of fungi. If fungus is present, a positive diagnosis is made.
Treatment
General: Fungal infections are treated with medications called antifungals. These medications cure the infection by destroying the fungi in the body. Depending on the type, severity, and location of the infection, as well as the patient's overall health, antifungals may be taken by mouth, applied to the skin, or injected into the vein. If a patient is infected with a different type of microorganism, such as a virus or a bacterium, antifungals will not be effective. Antifungals only work against fungi.
Safety: Some antifungal medications that are taken by mouth may cause liver damage. This is because they are strong medications that must be broken down by liver before they can be absorbed into the body. Ketoconazole (Nizoral®) and amphotericin B (Fungizone®, Abelcet®, AmBisome®, or Amphotec®) are the most likely to cause liver damage. Therefore, blood tests should be performed regularly during treatment to monitor liver function. Patients who experience nausea, vomiting, weakness, fatigue, abdominal pain (especially near the liver), dark urine, or jaundice (yellowing of the skin and eyes) should consult their healthcare providers immediately. These are all signs of liver damage.
According to the U.S. Food and Drug Administration (FDA), two oral antifungals, called itraconazole (Sporanox®) and terbinafine (Lamisil tablets®), have been associated with rare cases of liver failure and death. Itraconazole that is taken by mouth may weaken the heart and should not be prescribed for long-term use if a patient has a history of heart disease or heart failure.
Women who have symptoms of a yeast infection should consult their healthcare providers before taking over-the-counter medications. This ensures that the symptoms are caused by Candida albicans and not other microorganisms that cause sexually transmitted infections, such as gonorrhea or chlamydia.
Patients should tell their healthcare providers if they are taking any other drugs (prescription or over-the-counter), herbs, or supplements because they may interact with treatment. Patients should take medications exactly as prescribed.
Antifungal injections: Antifungal injections are typically used for severe fungal infections that affect multiple parts of the body. For instance, patients with disseminated histoplasmosis typically receive intravenous antifungals. Commonly used antifungal injections include amphotericin B (Amphocin® or Fungizone® Intravenous), flucytosine, voriconazole (Vfend®), and caspofungin (Cancidas®).
Antifungal suppositories: Vaginal yeast infections are treated with antifungal medications that are inserted directly into the vagina as suppositories. Common over-the-counter medications used include butoconazole (Femstat®), miconazole (Monistat 3®), and tioconazole (Vagistat® or Trosyd®).
Oral antifungals: Oral antifungals are used to treat a wide variety of fungal infections. For instance, patients with oral candidiasis (thrush) typically take nystatin suspension (Mycostatin®, Nilstat®, or Nystex®). Other antifungals that may be used to treat oral thrush include amphotericin B (Fungizone®), fluconazole (Diflucan®), and ketoconazole (Nizoral®).
Oral fluconazole (Diflucan®) may also be used to treat vulvovaginal candidiasis or yeast infection as an alternative to using antifungal creams.
Patients with fungal nail infections often take antifungals, such as terbinafine (Lamisil®), fluconazole (Diflucan®), or itraconazole (Sporanox®).
Patients who have athlete's foot that is not responding to over-the-counter medications may benefit from prescription-strength antifungals, such as itraconazole (Sporanox®), Fluconazole (Diflucan®), or terbinafine (Lamisil®).
Histoplasmosis is usually treated with antifungals, such as amphotericin B (Abelcet®) or itraconazole (Sporanox®). Treatment is continued until the fungus is killed. Patients with chronic pulmonary histoplasmosis and HIV patients who have weakened immune systems generally require lifelong treatment in order to prevent the infection from recurring.
Topical antifungals: Topical antifungals are medications that are applied to the skin to treat fungal infections. This includes creams, lotions, gels, powders, and shampoos. For instance, a cream called clotrimazole (Lotrimin®) is used to treat candidiasis infections of the vagina, mouth, and skin.
Patients with athlete's foot may use over-the-counter antifungal powders, creams, gels, or sprays such as terbinafine (Lamisil AT®), clotrimazole (Lotrimin AF®), or miconazole (Micatin®).
Jock itch (tinea cruris) is usually treated with over-the-counter lotions, powders, sprays, or gels such as terbinafine (Lamisil AT®), naftifine (Naftin®), miconazole (Micatin® or Monistat-Derm®), or clotrimazole (Lotrimin AF®). More severe cases that do not respond to treatment may require prescription-strength topical antifungals, such as econazole (Spectazole®) or oxiconazole (Oxistat®).
Shampoo that contains ketoconazole is often used to treat fungal infections of the scalp. Antifungal shampoos generally do not cause side effects.
Integrative Therapies
Good scientific evidence:
Zinc: Zinc formulations have been used since ancient Egyptian times to enhance wound healing. Evidence from human trials suggests that zinc pyrithione shampoo may be an effective treatment for tinea versicolor fungal infections of the scalp. Side effects were not noted. Additional research is needed before a strong recommendation can be made.
Zinc is generally considered safe when taken at the recommended dosages. Avoid zinc chloride since studies have not been done on its safety or effectiveness. While zinc appears safe during pregnancy in amounts lower than the established upper intake level, caution should be used since studies cannot rule out the possibility of harm to the fetus.
Unclear or conflicting scientific evidence:
Bishop's weed: Limited available human study used 8-methoxypsoralen (8-MOP), a photoreactive plant compound from bishopsweed, for the treatment of tinea versicolor. Clinical studies are needed before a conclusion can be made.
Use cautiously in patients with photosensitivity as bishop's weed may be photoreactive, and cause phototoxic skin damage, phototoxic dermatitis, and pigmentary retinopathy. Use cautiously in patients with bleeding disorders or taking anticoagulants, NSAIDs/anti-platelet agents, or herbs or supplements that increase risk of bleeding because bishop's weed may have additive effects and increase the risk of bleeding. Use cautiously in patients taking drugs or herbs or supplements metabolized by cytochrome P450 as bishop's weed may increase the effects of these agents. Use cautiously in patients with eye disorders, as bishop's weed may cause ocular toxicity. Avoid in patients with known allergy/hypersensitivity to bishop's weed, its constituents, or members of the Apiaceae family.
Bitter orange: Limited available human study found promising results using the oil of bitter orange for treatment of fungal infections. However, due to methodological weakness of this research, further evidence is needed to confirm these results.
Avoid if allergic or hypersensitive to bitter orange or any members of the Rutaceae family. Avoid with heart disease, narrow-angel glaucoma, intestinal colic, or long QT interval syndrome. Avoid if taking anti-adrenergic agents, beta-blockers, QT-interval prolonging drugs, monoamine oxidase inhibitors (MAOIs), stimulants, or honey. Use cautiously with headache, hyperthyroidism (overactive thyroid), or if fair-skinned. Avoid if pregnant or breastfeeding.
Cinnamon: There is currently a lack of available evidence to support the use of cinnamon for AIDS patients with advanced oral candidiasis. More study is needed in this area.
Avoid if allergic or hypersensitive to cinnamon, its constituents, members of the Lauraceae family, or Balsam of Peru. Use cautiously if prone to atopic reactions or if taking cytochrome P450 metabolized agents, anticoagulants (blood thinners), insulin or blood sugar-altering medications, antibiotics, or cardiovascular agents. Avoid if pregnant or breastfeeding.
Cranberry: Limited laboratory research has examined the antifungal activity of cranberry. Reliable human studies supporting the use of cranberry for fungal infections are currently lacking. Further research is warranted in this area.
Avoid if allergic to cranberries, blueberries, or other plants of the Vaccinium species. Sweetened cranberry juice may affect blood sugar levels. Use cautiously with a history of kidney stones. Pregnant and breastfeeding women should avoid cranberry in higher amounts than what is typically found in foods.
Garlic: Garlic is used both medicinally and as a food spice. Several studies describe the use of garlic as a topical antifungal to treat fungal infections of the skin, including yeast infections. More research is needed in this area.
Use cautiously as garlic can cause severe burns and rash when applied to the skin of sensitive individuals. Avoid if allergic or hypersensitive to garlic or other members of the Lilaceae(lily) family (e.g. hyacinth, tulip, onion, leek, or chive). Avoid with a history of bleeding problems, asthma, diabetes, low blood pressure, or thyroid disorders. Stop using supplemental garlic two weeks before and immediately after dental/surgical/diagnostic procedures with bleeding risks. Avoid in supplemental doses if pregnant or breastfeeding.
Pomegranate: In clinical study, an extract of pomegranate was shown to be as effective as a commonly used oral gel when used topically to treat candidiasis associated with denture stomatitis (mouth sores). Additional study is needed to confirm pomegranate's antifungal effects.
Avoid if allergic or hypersensitive to pomegranate. Avoid with diarrhea or high or low blood pressure. Avoid taking pomegranate fruit husk with oil or fats to treat parasites. Pomegranate root/stem bark should only be used under the supervision of a qualified healthcare professional. Use cautiously with liver damage or liver disease. Pomegranate supplementation may be unsafe during pregnancy when taken by mouth. The bark, root, and fruit rind may cause menstruation or uterine contractions. Avoid if breastfeeding due to a lack of scientific data.
Probiotics: Early research suggests that cheese containing probiotics may help reduce the risk of a fungal mouth infection, called thrush, in the elderly. More research is needed in this area.
Probiotics are generally considered to be safe and well-tolerated. Avoid if allergic or hypersensitive to probiotics. Use cautiously if lactose intolerant. Caution is advised when using probiotics in neonates born prematurely or with immune deficiency.
Propolis: Propolis is a natural resin created by bees to make their hives. Propolis is made from the buds of conifer and poplar trees and combined with beeswax and other bee secretions. In human study, a commercial propolis ethanol extract from Brazil, formulated to ensure physical and chemical stability, was found to inhibit fungal infections of the mouth, such as oral candidiasis. Additional research is needed to confirm these findings.
Avoid if allergic or hypersensitive to propolis, black poplar (Populas nigra), poplar bud, bee stings, bee products, honey, or Balsam of Peru. Severe allergic reactions have been reported. There has been one report of kidney failure with the ingestion of propolis that improved upon discontinuing therapy and deteriorated with re-exposure. Avoid if pregnant or breastfeeding because of the high alcohol content in some products.
Seaweed, kelp, bladderwrack: Bladderwrack (Fucus vesiculosus) is a brown seaweed found along the northern coasts of the Atlantic and Pacific oceans and North and Baltic seas. Another seaweed that grows alongside bladderwrack is Ascophyllum nodosum, andit is often combined with bladderwrack in kelp preparations. Laboratory research suggests that bladderwrack may have antifungal activity. However, reliable human studies to support this use are currently lacking in the available literature.
Avoid if allergic or hypersensitive to Fucus vesiculosus or iodine. Avoid with a history of thyroid disease, bleeding, acne, kidney disease, blood clots, nerve disorders, high blood pressure, stroke, or diabetes. Avoid if pregnant or breastfeeding.
Selenium: Selenium is a mineral found in soil, water, and some foods. Commercially available 1% selenium sulfide shampoo has been reported as equivalent to sporicidal therapy in the adjunctive treatment of the yeast infection tinea capitis. However, further high-quality evidence is warranted.
Selenium sulfide shampoo has also been studied as a possible treatment for tinea versicolor. However, research results are inconclusive.
Avoid if allergic or hypersensitive to products containing selenium. Avoid with a history of non-melanoma skin cancer. Selenium is generally regarded as safe for pregnant or breastfeeding women. However, animal research reports that large doses of selenium may lead to birth defects.
Tea tree oil: Although tea tree oil has been found to have activity against several fungus species in laboratory study, there is currently insufficient human evidence to determine if it is an effective topical treatment for onychomycosis, tinea pedis (athlete's foot), or thrush (oral Candida albicans).
Tea tree oil may be toxic when taken by mouth and therefore, should not be swallowed. Avoid if allergic to tea tree oil or plants of the Myrtle (Myrtaceae) family, Balsam of Peru, or benzoin. Use cautiously with a history of eczema. Avoid if pregnant or breastfeeding.
Thyme: Thyme has been used medicinally for thousands of years. Beyond its common culinary application, it has been recommended for many indications based on proposed antimicrobial, antitussive, spasmolytic, and antioxidant activity. Thyme essential oil and thymol have been shown to have antifungal effects. Topical thymol has been used traditionally to treat paronychia (skin infection around a finger or toenail) and onycholysis (fungal nail infection). Currently, there is insufficient reliable human evidence to recommend for or against the use of thyme or thymol as a treatment for fungal infections.
Avoid if allergic or hypersensitive to thyme, members of the Lamiaceae (mint) family, any component of thyme, or rosemary (Rosmarinus officinalis). Avoid oral ingestion or non-diluted topical application of thyme oil due to potential toxicity. Avoid topical preparations in areas of skin breakdown or injury or in atopic patients due to multiple reports of contact dermatitis. Use cautiously with gastrointestinal irritation or peptic ulcer disease due to anecdotal reports of gastrointestinal irritation. Use cautiously with thyroid disorders due to observed anti-thyrotropic effects in animal research of the related species Thymus serpyllum. Avoid if pregnant or breastfeeding.
Prevention
Practicing good hygiene and regularly washing the hands with soap and water may help reduce the risk of acquiring infections. This is especially important after exposure to soil (e.g. gardening) because many types of fungi live in the dirt. Good hygiene may also reduce the risk of passing a contagious infection on to others.
Fungi prefer warm, moist environments. Therefore, patients should limit their exposure to such conditions. Individuals should wear shower shoes (e.g. flip flops or sandals) when they are exposed to wet or moist surfaces at a public setting. This includes public showers and swimming pools at gyms and workout clubs. Patients should change their socks if they become sweaty. Individuals, especially those who are obese, should carefully dry themselves after taking a shower.
All produce should be washed thoroughly before eating to prevent exposure to disease-causing organisms, such as Histoplasma capsulatum.This is because produce is grown in the soil, which is a common habitat for fungi.
Author Information
This information has been edited and peer-reviewed by contributors to the Natural Standard Research Collaboration (www.naturalstandard.com).
Bibliography
Natural Standard developed the above evidence-based information based on a thorough systematic review of the available scientific articles. For comprehensive information about alternative and complementary therapies on the professional level, go to www.naturalstandard.com. Selected references are listed below.
Alvarez MS, Silverberg NB.Tinea capitis. Cutis. 2006 Sep;78(3):189-96. View Abstract.
American Dermatological Association. www.amer-derm-assn.org.
Centers for Disease Control and Prevention (CDC). www.cdc.gov.
Krause R, Krejs GJ, Wenisch C, et al. Elevated fecal Candida counts in patients with antibiotic-associated diarrhea: role of soluble fecal substances. Clin Diagn Lab Immunol. 2003 Jan;10(1):167-8. View Abstract.
Maslak P, Southern L. Histoplasmosis.Blood. 2007 Apr 1;109(7):2677. View Abstract.
National Institutes of Health (NIH). www.nih.gov.
Natural Standard: The Authority on Integrative Medicine. www.naturalstandard.com.
Seebacher C, Abeck D, Brasch J, et al. Tinea capitis: ringworm of the scalp. Mycoses. 2007 May;50(3):218-26. View Abstract.
Sobel JD. Vulvovaginal candidosis.Lancet. 2007 Jun 9;369(9577):1961-71. View Abstract.
Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998 Feb;178(2):203-11. View Abstract.
U.S. Food and Drug Administration (FDA). www.fda.gov.
Vender RB, Lynde CW, Poulin Y.Prevalence and epidemiology of onychomycosis. J Cutan Med Surg. 2006 Dec;10 Suppl 2:S28-33. View Abstract.
Copyright © 2013 Natural Standard (www.naturalstandard.com)
The information in this monograph is intended for informational purposes only, and is meant to help users better understand health concerns. Information is based on review of scientific research data, historical practice patterns, and clinical experience. This information should not be interpreted as specific medical advice. Users should consult with a qualified healthcare provider for specific questions regarding therapies, diagnosis and/or health conditions, prior to making therapeutic decisions.
Updated:
March 22, 2017