Esophagitis
Esophagitis
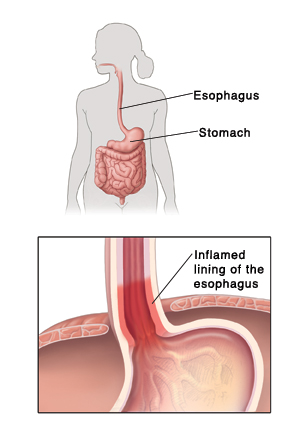
Do you often have burning pain in your chest? You may have esophagitis. This is when the lining of the esophagus becomes red and swollen (inflamed). The esophagus is the tube that connects your throat to your stomach. This sheet tells you more about esophagitis. It also explains your treatment options.
Main types of esophagitis
Reflux esophagitis. This is the more common type. It is caused by GERD (gastroesophageal reflux disease). Stomach contents with stomach acid flow back up into the esophagus. This happens over and over. It leads to inflammation. Risk factors can include:
Being overweight
Asthma
Smoking
Pregnancy
Frequent vomiting
Certain medicines (such as aspirin and other anti-inflammatories)
Hiatal hernia
Infectious esophagitis. This is caused by an infection. You are more at risk for this if you have a weakened immune system and poor nutrition. Antibiotic use can also be a factor. The infection is often due to the following:
A type of fungus (typically candida)
A virus, such as herpes simplex virus 1 (HSV-1) or cytomegalovirus (CMV)
Eosinophilic esophagitis. Foods or other things around you can give you an allergic reaction. This triggers an immune response and leads to esophagitis.
Pill-induced esophagitis. Certain types of medicines can cause inflammation and ulcers in the esophagus. These include doxycycline, aspirin, NSAIDs, alendronate, potassium, quinidine, iron.
Symptoms of esophagitis
The following symptoms can occur with esophagitis:
Pain when swallowing, or trouble swallowing
Pain behind your breastbone (heartburn)
Acid regurgitation
Chronic sore throat
Gum Inflammation
Cavities
Bad breath
Nausea
Pain in your upper belly (abdomen)
Bleeding (indicated by bright red vomit or black, tarry stool)
These symptoms occur more often with reflux esophagitis:
Coughing, wheezing, or asthma
Hoarseness
Diagnosis of esophagitis
Your healthcare provider will ask about your health history and symptoms. You’ll also be examined. Sometimes certain tests are needed. These may include:
Upper endoscopy. A thin, flexible tube with a tiny light and camera is used. It is inserted through the mouth down into the esophagus. This lets the provider look for damage. A small sample of tissue (biopsy) may also be removed. The sample is sent to a lab for testing.
Upper GI X-ray with barium. An X-ray is done after you drink a substance called barium. Barium may make problems in the esophagus easier to see on an x-ray.
Esophageal pH. A soft, thin tube is passed into the esophagus through the nose or mouth for 24 hours. It measures the acid level in the esophagus.
Esophageal manometry. A soft, thin tube is passed into the esophagus through the nose or mouth. It measures muscle contractions in the esophagus.
Treatment of esophagitis
Medicines. Different medicines can help treat esophagitis. The medicine used will depend on the type of esophagitis you have. Talk with your healthcare provider.
Lifestyle changes. Making the following changes can help reduce irritation and ease your symptoms:
Avoid spicy foods (pepper, chili powder, curry). Also avoid hard foods (nuts, crackers, raw vegetables) and acidic foods and drinks (tomatoes, citrus fruits and juices). Other problem foods include chocolate, peppermint, nutmeg, and foods high in fat.
Until you can swallow without pain, follow a combined liquid and soft diet. Try foods such as cooked cereals, mashed potatoes, and soups.
Take small bites and chew your food thoroughly.
Avoid large meals and heavy evening meals. Don't lie down within 2 to 3 hours of eating.
Get to or stay at a healthy weight.
Avoid alcohol, caffeine, and smoking or tobacco products.
Brush and floss your teeth
Raise your upper body by 4 to 6 inches when lying in bed. This can be done using a foam wedge. Or put blocks under the legs at the head of your bed.
Surgery. This may be needed for severe reflux esophagitis. Other noninvasive procedures to treat GERD and esophagitis are being studied. Your provider can tell you more.
Why treatment Is important
Without treatment, esophagitis can get worse. This is especially true with severe reflux esophagitis. For instance, continued symptoms can cause scarring of the esophagus. Over time, this can cause a narrowing the esophagus (stricture). This can make it hard to pass food down to the stomach. As symptoms go on they can also cause changes in the lining of the esophagus. These changes can put you at a slightly higher risk of cancer of the esophagus.
Updated:
March 21, 2017
Sources:
Medication-induced esophagitis. UpToDate
Reviewed By:
Fraser, Marianne, MSN, RN,Lehrer, Jenifer, MD