Cerebral Aneurysm
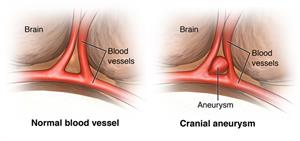
A cerebral aneurysm (also called an intracranial aneurysm or brain aneurysm) is a bulging, weakened area in the wall of an artery in the brain, resulting in an abnormal ballooning of the artery that is at risk for rupturing. A cerebral aneurysm more often happens in an artery located in the front part of the brain that supplies oxygen-rich blood to the brain tissue. Arteries anywhere in the brain can develop aneurysms. A normal artery wall is made up of 3 layers. The wall where the aneurysm forms is thin and weak because of an abnormal loss or absence of the muscular layer of the artery wall, leaving only 2 layers. There are several types of aneurysms:
- Berry aneurysm. The most common type of cerebral aneurysm is called a saccular, or berry, aneurysm, happening in 90% of cerebral aneurysms. This type of aneurysm looks like a "berry" with a narrow stem. More than one aneurysm may be present.
- Fusiform aneurysm. A fusiform aneurysm bulges out on all sides. This forms a dilated artery. Fusiform aneurysms are often associated with atherosclerosis.
- Dissecting aneurysm. A dissecting aneurysm results from a tear along the length of the artery in the inner layer of the artery wall, causing blood to leak in between the layers of the wall. This may cause a ballooning out on one side of the artery wall, or it may block off or obstruct blood flow through the artery. Dissecting aneurysms usually happen from traumatic injury, but they can also happen spontaneously. The shape and location of the aneurysm may determine which treatment is recommended.
Most cerebral aneurysms present without any symptoms and are small in size (less than 10 millimeters, or less than four-tenths of an inch, in diameter). Smaller aneurysms may have a lower risk of rupture.
Currently, the cause of cerebral aneurysms is not clearly understood. Brain aneurysms are associated with several factors. This includes smoking, high blood pressure, and family history (genetic). The ultimate cause of a brain aneurysm is an abnormal breaking down and weakening in the wall of an artery, and the effects of pressure from the pulsations of blood being pumped forward through the arteries in the brain. Certain locations of an aneurysm may create greater pressure on the aneurysm, such as the area where the artery divides into smaller branches.
Inherited risk factors associated with aneurysm formation may include the following:
- Alpha-glucosidase deficiency. A complete or partial deficiency of the enzyme needed to break down glycogen and to convert it into glucose.
- Alpha 1-antitrypsin deficiency. A hereditary disease that may lead to hepatitis and cirrhosis of the liver or emphysema of the lungs.
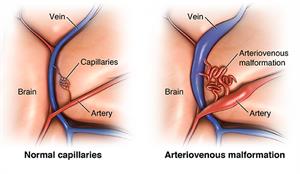
- Arteriovenous malformation (AVM). An abnormal connection between an artery and a vein.
- Coarctation of the aorta. A narrowing of the aorta. This is the main artery coming from the heart.
- Ehlers-Danlos syndrome. A connective tissue disorder (less common).
- Family history of aneurysms
- Female gender
- Fibromuscular dysplasia. An arterial disease, cause unknown, that most often affects the medium and large arteries of young to middle-aged women.
- Hereditary hemorrhagic telangiectasia. A genetic disorder of the blood vessels in which there is a tendency to form blood vessels that lack capillaries between an artery and vein.
- Klinefelter syndrome. A genetic condition in men in which an extra X sex chromosome is present.
- Noonan's syndrome. A genetic disorder that causes abnormal development of many parts and systems of the body.
- Polycystic kidney disease (PCKD). A genetic disorder characterized by the growth of numerous cysts filled with fluid in the kidneys. PCKD is the most common medical disease associated with saccular aneurysms.
- Tuberous sclerosis. A type of neurocutaneous syndrome that can cause tumors to grow inside the brain, spinal cord, organs, skin, and skeletal bones.
Acquired risk factors associated with aneurysm formation may include the following:
- Advancing age
- Alcohol consumption (especially binge drinking)
- Atherosclerosis. A buildup of plaque (made up of deposits of fatty substances, cholesterol, cellular waste products, calcium, and fibrin) in the inner lining of an artery
- Cigarette smoking
- Use of illicit drugs, such as cocaine or amphetamine
- High blood pressure
- Head injury
- Infection
Although these risk factors increase a person's risk, they do not necessarily cause the disease. Some people with one or more risk factors never develop the disease, while others develop disease and have no known risk factors. Knowing your risk factors to any disease can help to guide you into the appropriate actions. These include changing behaviors and being monitored for the disease.
The presence of a cerebral aneurysm may not be known until it ruptures. Most cerebral aneurysms have no symptoms and are small in size (less than 10 millimeters, or less than four-tenths of an inch, in diameter). Smaller aneurysms may have a lower risk of rupture.
However, occasionally there may be symptoms that happen before a rupture due to a small amount of blood that may leak. This is called "sentinel hemorrhage" into the brain. Some aneurysms are symptomatic because they press on adjacent structures, such as nerves to the eye. They can cause visual loss or diminished eye movements, even if the aneurysm has not ruptured.
The symptoms of an unruptured cerebral aneurysm include the following:
- Headaches (rare, if unruptured)
- Eye pain
- Vision changes
- Diminished eye movement
The first evidence of a cerebral aneurysm is most often a subarachnoid hemorrhage (SAH), due to rupture of the aneurysm. This may cause symptoms such as:
- Rapid onset of "worst headache of my life"
- Stiff neck
- Nausea and vomiting
- Changes in mental status, such as drowsiness
- Pain in specific areas, such as the eyes
- Dilated pupils
- Loss of consciousness
- High blood pressure
- Loss of balance or coordination
- Sensitivity to light
- Back or leg pain
- Problems with certain functions of the eyes, nose, tongue, and/or ears that are controlled by one or more of the 12 cranial nerves
- Coma and death
The symptoms of a cerebral aneurysm may resemble other problems or medical conditions. Always talk with your healthcare provider for a diagnosis.
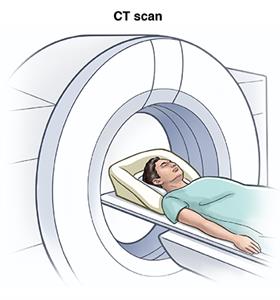
A cerebral aneurysm is often discovered after it has ruptured or by chance during diagnostic exam, such as computed tomography (CT scan), magnetic resonance imaging (MRI), or angiography that are being done for other reasons.
In addition to a complete medical history and physical exam, diagnostic procedures for a cerebral aneurysm may include:
- Cerebral angiography. This provides an image of the blood vessels in the brain to detect a problem with vessels and blood flow. The procedure involves inserting a catheter (a small, thin tube) into an artery in the leg and passing it up to the blood vessels in the brain. Contrast dye is injected through the catheter and X-ray images are taken of the blood vessels.
- Computed tomography scan (CT or CAT scan). This is an imaging test that uses X-rays and a computer to make detailed images of the body. A CT scan shows details of the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays and may be used to detect abnormalities and help identify the location of the aneurysm and if it has burst or is leaking. A CT angiogram (CTA) can also be obtained on a CT scan to look at the vessels.
- Magnetic resonance imaging (MRI). A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. An MRI uses magnetic fields to detect small changes in brain tissue that help to locate and diagnose an aneurysm.
- Magnetic resonance angiography (MRA). A noninvasive diagnostic procedure that uses a combination of magnetic resonance technology (MRI) and intravenous (IV) contrast dye to visualize blood vessels. Contrast dye causes blood vessels to appear opaque on the MRI image, allowing the doctor to visualize the blood vessels being evaluated.
Your healthcare provider will figure out the best treatment for you based on:
- How old you are
- Your overall health and past health
- How sick you are
- How well you can handle specific medicines, procedures, or therapies
- How long the condition is expected to last
- Your opinion or preference
Depending on your situation, the healthcare provider will make recommendations for the intervention that is appropriate. Whichever intervention is chosen, the main goal is to decrease the risk of subarachnoid hemorrhage, either initially or from a repeated episode of bleeding.
Many factors are considered when making treatment decisions for a cerebral aneurysm. The size and location of the aneurysm, the presence or absence of symptoms, the person’s age and medical condition, and the presence or absence of other risk factors for aneurysm rupture are considered. In some cases, the aneurysm may not be treated and the person will be closely followed by a healthcare provider. In other cases, surgical treatment may be indicated.
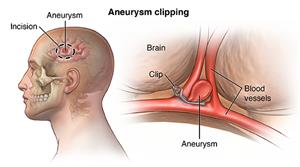
There are two primary surgical treatments for a cerebral aneurysm:
- Open craniotomy (surgical clipping). This procedure involves the surgical removal of part of the skull. The healthcare provider exposes the aneurysm and places a metal clip across the neck of the aneurysm to prevent blood flow into the aneurysm sac. Once the clipping is completed, the skull is secured back together.
- Endovascular coiling or coil embolization. Endovascular coiling is a minimally invasive technique. This means an incision in the skull is not needed to treat the cerebral aneurysm. Rather, a catheter is advanced from a blood vessel in the groin up into the blood vessels in the brain. Fluoroscopy (live X-ray) will be used to assist in advancing the catheter into the head and into the aneurysm. Once the catheter is in place, very tiny platinum coils are advanced through the catheter into the aneurysm. These tiny, soft, platinum coils, which are visible on X-ray, conform to the shape of the aneurysm. The coiled aneurysm becomes clotted off (embolization), preventing rupture. This procedure is performed either under general or local anesthesia.
Although a cerebral aneurysm may be present without symptoms, the most common initial symptom of a cerebral saccular aneurysm is a sudden headache from a subarachnoid hemorrhage (SAH) or bleeding in the space between the brain and the membranes that cover the brain. Minor subarachnoid hemorrhage most often happens after head injury. Major subarachnoid hemorrhage is most commonly from a ruptured cerebral saccular aneurysm. A sudden headache associated with SAH is a medical emergency.
Increased risk for aneurysm rupture is associated with aneurysms that are over 10 millimeters (less than four-tenths of an inch) in diameter, in a particular location (circulation in the back portion of the brain), and/or previous rupture of another aneurysm. A significant risk of death is associated with the rupture of a cerebral aneurysm.
Hemorrhagic strokes happen when a blood vessel that supplies the brain ruptures and bleeds. When an artery bleeds into the brain, brain cells and tissues do not receive oxygen and nutrients. In addition, pressure builds up in surrounding tissues and irritation and swelling happens. About 20% of strokes are caused by hemorrhagic bleeding.
Controlling your risk factors may decrease your risk of having an aneurysm. These risk factors include:
- Alcohol consumption (especially binge drinking)
- Atherosclerosis
- Obesity
- Cigarette smoking
- Use of illicit drugs, such as cocaine or amphetamine
- High blood pressure
- Head injury
- Infection
Although these risk factors increase a person's risk, they do not necessarily cause the disease. Some people with one or more risk factors never develop the disease. Others develop the disease and have no known risk factors. Knowing your risk factors to any disease can help to guide you into the appropriate actions. These include changing behaviors and being clinically monitored for the disease.
Any person experiencing some or all of the following symptoms, regardless of age, should undergo immediate and careful evaluation by a healthcare provider:
- Headache located in one place
- Dilated pupils
- Blurred or double vision
- Pain above and behind either eye
- Weakness and numbness
- Difficulty speaking
Ruptured brain aneurysms usually result in a subarachnoid hemorrhage (SAH). This is defined as bleeding into the space around the brain called the subarachnoid space. A SAH can be life-threatening.
You should seek medical attention immediately if you are experiencing some or all of these symptoms:
- Sudden severe headache or "the worst headache of your life”
- Loss of consciousness
- Nausea and/or vomiting
- Stiff neck
- Sudden blurred or double vision
- Sudden pain above or behind the eye or trouble seeing
- Sudden change in mental status or awareness
- Sudden trouble walking or dizziness
- Sudden weakness and numbness
- Sensitivity to light known as photophobia
- Seizure activity
- Drooping eyelid
- A cerebral aneurysm (also called an intracranial aneurysm or brain aneurysm) is a bulging, weakened area in the wall of an artery in the brain. This results in an abnormal widening, ballooning, or bleb.
- Because there is a weakened spot in the aneurysm wall, there is a risk for rupture (bursting) of the aneurysm.
- You should seek medical attention immediately if you are experiencing some or all of these symptoms:
- Sudden severe headache or "the worst headache of your life”
- Loss of consciousness
- Nausea and/or vomiting
- Stiff neck
- Sudden blurred or double vision
- Sudden pain above or behind the eye or trouble seeing
- Sudden change in mental status or awareness
- Sudden trouble walking or dizziness
- Sudden weakness and numbness
- Sensitivity to light known as photophobia
- Seizure activity
- Drooping eyelid
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Updated:
April 03, 2018
Reviewed By:
Shelat, Amit, MD,Dozier, Tennille, RN, BSN, RDMS