Thrombolytic Therapy for Stroke
Thrombolytic Therapy for Stroke
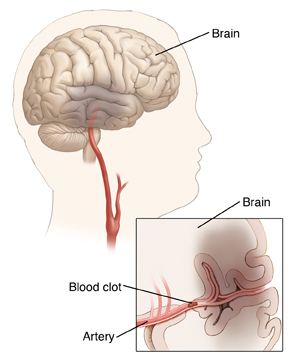
An ischemic stroke occurs when blood flow to the brain is blocked. This is most often because of a blood clot in an artery in the brain or artery leading to the brain. Treatment is needed right away to help dissolve the clot and restore normal blood flow. Restoring normal blood flow can limit damage to brain tissue and improve outcome. With thrombolytic therapy, a clot-busting medicine called tissue plasminogen activator or tPA is used to dissolve the clot.
Before the treatment
People with certain health problems have increased risks of problems with thrombolytic therapy. For this reason, a detailed health history must be taken to check whether it is safe to have the treatment. Be sure to tell your healthcare provider about any health problems you have. The provider will also ask whether you’ve had specific problems, such as a prior stroke, head injury, and bleeding in the brain.
Tell the healthcare provider about all medicines you take. Be sure to mention if you take blood thinners (anticoagulants). Also mention if you take over-the-counter medicines, herbal medicines, and other supplements.
Tell your healthcare provider about the use of any alcohol or tobacco products so that he or she can provide you with the safest possible care.
Tell your healthcare provider if you are pregnant or if you have had recent surgery or head injury.
Certain tests need to be done before the treatment. These include blood tests and imaging tests, such as a CT or MRI scan of the brain.
During the treatment
The treatment is done using an IV line. This is a small tube that is put in a vein in the hand or arm. Clot-busting medicine is sent through the IV line to reach the clot. The medicine is delivered continuously for one or more hours. You’ll be monitored closely throughout the treatment.
After the treatment
Following the treatment, you’ll need to stay in the hospital for several days or longer. More imaging tests will be done to check how well the clot is dissolving. Other tests may also be done to help find the cause of the stroke.
Risks and possible complications
Bleeding in the brain or elsewhere in the body
Allergic reaction to the clot-busting medication (skin rash, itching, swelling of your face or tongue)
Chest pain or pressure
Severe headache
Shortness of breath
Worsening of heart problems
Dizziness or lightheadedness
Nausea and vomiting
Death
Follow-up care
Recovery from a stroke can take several months or longer. Be sure to keep all follow-up appointments with your doctor. These are needed to monitor your health and the progress of your recovery. Other treatments, such as medicines, rehabilitation, and surgery, may be needed in the future. Your healthcare provider will discuss these with you as needed.
Call 911
Call 911 or go to an emergency room (ER) right away if you have any of the following signs of a stroke:
Sudden, unexplained numbness or weakness on one side of the body
Problems seeing, double vision, or blurry vision
Sudden confusion or problems with speech
Sudden dizziness, trouble walking, or problems with balance
Sudden, severe headache
Think F.A.S.T.
F.A.S.T. is an easy way to remember the signs of a stroke. When you see these signs, you will know that you need to call 911 fast.
F.A.S.T. stands for:
F is for face drooping. One side of the face droops or is numb. When the person smiles, the smile is uneven.
A is for arm weakness, One arm is weak or numb. When the person lifts both arms at the same time, one arm may drift downward.
S is for speech difficulty. You may notice slurred speech or difficulty speaking. The person can't repeat a simple sentence correctly when asked.
T is for time to call 911. If someone shows any of these symptoms, even if they go away, call 911 right away. Make note of the time the symptoms first appeared.
If you are at risk for having a stroke:
Keep a list of important phone numbers next to your phone or in your cell phone list of contacts. Include your doctor and relatives or friends you want to be contacted.
Carry a list of all medicines you take and the dosages of each, in your wallet. Include over-the-counter medicines, vitamins, and supplements.
Write a brief health history, including any other medical problems you have had and the dates. Keep this with the medicine list.
Updated:
August 08, 2018
Sources:
Intravenous fibrinolytic (thrombolytic) therapy in acute ischemic stroke: Therapeutic use, Up To Date
Reviewed By:
Image reviewed by StayWell medical illustration team.,Sudheendra, Deepak, MD,Turley, Ray, BSN, MSN