Understanding Vulvectomy
Understanding Vulvectomy
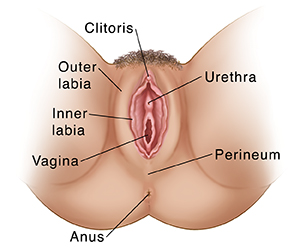
The vulva area has several parts. These include the inner and outer labia, and the clitoris. The vulva area also includes the opening of the vagina and the opening of the urinary tract (urethra).
The surgery can be done in many ways. It depends in part on how much tissue needs to be removed. The surgeon may remove an area of skin from only the outer part of the labia. Or the surgeon may remove some or all of the outer and inner labia. In many cases, the clitoris is left in place. In some cases, more tissue may be removed. In rare cases, the surgeon may do a radical vulvectomy. This surgery removes a large area of tissue, including parts of the inside of the upper thighs, lower belly, and the area between the vagina and anus (perineum). The surgeon may also remove small glands (lymph nodes) in the groin.
How to say it
vuhl-VEK-tuh-mee
Why vulvectomy is done
The surgery may be done to treat conditions such as:
Cancer of the vulva
Precancer of the vulva (vulvar intraepithelial neoplasia)
Skin cancer (melanoma) on the vulva
Severe skin disease, such as lichen sclerosus
Severe disease of sweat glands in the groin (hidradenitis suppurativa)
The surgery may be done if you cannot have another treatment such as ablation, or that treatment hasn’t cured the problem.
How vulvectomy is done
If you have gone through menopause, your healthcare provider may have you use estrogen cream for several weeks before surgery. This is to help make the skin in the area healthier for surgery.
During the surgery:
You lie on a medical table. You are given medicine to relax you or make you sleep through the procedure. You may be numbed from the waist down.
The surgeon cuts away the area of diseased tissue. He or she also removes a small amount of additional tissue around the area. This is to help make sure all the diseased tissue is gone. The surgeon will remove layers of tissue that may include the fat under the skin.
The surgeon may bring together edges of the skin and close them with stitches (sutures). The surgeon may use flaps of skin to close some areas. Small of patches healthy skin may be left to create new tissue. In some cases, the surgeon may use a skin graft. That means an area of healthy skin is taken from another part of the body. The skin graft is then stitched in place over the parts of the vulva that need to be covered.
The surgeon covers the area with a dressing to protect it and help it heal. If a skin graft was done, the donor site may also be covered.
You will likely have a thin, flexible tube (catheter) in your urethra and bladder for up to a week. This is to help drain urine from your bladder while you heal.
While you heal from the surgery, you may need to avoid certain activities. You may need bed rest for a period of time. After bed rest, you may be told to not climb stairs and to limit your walking. You may also need to keep your legs close together. This is to help the incisions heal.
Risks of vulvectomy
Infection
Scarring
Changes in sexual function and body image
Need for more surgery to remove more tissue
Blood clot from bed rest
Excess bleeding
Blood blister under the skin (hematoma)
Incisions that separate
Updated:
March 21, 2017
Sources:
Baggish MS. Vulvectomy. In: Baggish MS, editor. Atlas of Pelvic Anatomy and Gynecologic Surgery. 4 ed. Phildelphia: Elsevier; 2016. p. 909-28., Helm CW. Radical vulvectomy. Up To Date. January 22 ed: Up To Date; 2016. p. 32., Helm CW. Vulvar wide local excision, simple vulvectomy, and skinning vulvectomy. Up To Date. January 26 ed: Up To Date; 2016. p. 17., Polgar Bailey P. Vulvar and Vaginal Disorders In: Buttaro TM, editor. Primary Care. 4 ed. Philadelphia: Mosby; 2013. p. 874-86.
Reviewed By:
Burd, Irina, MD, PhD,Image reviewed by StayWell medical illustration team.,Ziegler, Olivia, MS, PA